The condition probably results from stasis or obstruction in the narrow neck of a diverticulum, which, in turn, leads to an overgrowth of bacteria. The principal micro-organisms isolated from affected patients are anaerobes, gram-negative aerobes, and some facultative gram-positive bacteria.
Range of severity can be wide
Presentation of diverticulitis may range in severity from mild to moderate lower abdominal pain associated with anorexia, nausea, and vomiting to abscess and fistula formation, colonic stricture, bowel obstruction, and peritonitis (“complicated diverticulitis”). Peritonitis may arise from rupture of a peridiverticular abscess or free rupture of an uninflamed diverticulum. Diverticulitis may be particularly severe in immunocompromised patients.
Classification of disease
The most accepted classification system for diverticulitis is the Hinchey system:
- in stage 1 disease, patients have small and confined pericolic or mesenteric abscesses
- in stage 2, the abscesses are larger but usually remain confined to the pelvis
- in stage 3, an abscess ruptures and causes purulent peritonitis
- stage 4 disease is distinguished by rupture of an uninflamed and unobstructed diverticulum (known as “free rupture”); this stage has the highest risk of adverse outcomes.
CT is best for diagnosis
The most useful diagnostic test for diverticulitis is a computed tomography (CT) scan. As a general rule, endoscopy should be avoided because of the risk of intestinal perforation.
Most patients can be treated as outpatients
Patients who have mild disease usually can be treated as outpatients. They should receive a 7- to 10-day course of oral antibiotics such as ciprofloxacin, 500 to 750 mg every 12 hours, plus metronidazole, 500 mg every 6 to 8 hours.
Alternate oral regimens include metronidazole, 500 mg every 6 to 8 hours, plus trimethoprim-sulfamethoxazole, double-strength, every 12 hours, or amoxicillin-clavulanate, 875 mg every 12 hours.
For seriously ill patients, hospitalization is warranted
Seriously ill patients—particularly those who are immunocompromised—should be hospitalized. If bowel obstruction is present, a nasogastric tube should be inserted. Appropriate IV antibiotic regimens for hospitalized patients include:
- metronidazole, 500 mg every 6 to 8 hours, plus ciprofloxacin, 400 mg every 12 hours
- metronidazole, 500 mg every 6 to 8 hours, plus ceftriaxone, 1 to 2 g every 24 hours
- ampicillin–sulbactam, 3 g every 6 hours
- piperacillin–tazobactam, 3.375 g every 6 hours
- ticarcillin–clavulanate, 3.1 g every 6 hours.
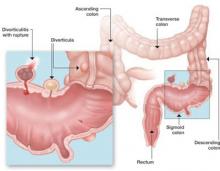
FIGURE 3 Consider diverticulitis in older women who complain of acute abdominal pain
Diverticulitis generally affects the sigmoid colon and descending colon and probably arises from stasis or obstruction in the narrow neck of a diverticulum, which leads to an overgrowth of bacteria and possible rupture.If an abscess is present and fails to respond promptly to medical therapy, drainage may be necessary. Some abscesses can be drained percutaneously under CT guidance. Large abscesses, in association with signs of generalized peritonitis, uncontrolled sepsis, or intestinal perforation, require surgical intervention, either via laparoscopy or open laparotomy. Preliminary data suggest that the laparoscopic approach may result in a shorter hospital stay, decreased postoperative pain, and an overall reduced rate of perioperative complication.
Diverticulitis may mimic appendicitis
The clinical presentation of diverticulitis is similar to that of appendicitis, except that the pain is usually on the left. Perforation, with resulting peritonitis, is an ever-present and potentially life-threatening complication. The dominant organisms are anaerobes and coliforms. The best diagnostic test is CT.
Patients in the early stages of disease can usually be treated as outpatients with antibiotics that are quite familiar to all ObGyns— i.e., metronidazole and a quinolone. More seriously ill patients should be hospitalized and treated with IV antibiotics and nasogastric suctioning.
Consultation with an interventional radiologist and general surgeon is recommended if operative intervention is necessary.