In a pooled analysis of the two studies of the contraceptive patch by Jick and colleagues and the one study by Cole and associates, the overall and method failure rates through 13 cycles were 0.8% and 0.6%, respectively, representing 15 pregnancies.1
Subject weights were divided into deciles to determine the number of pregnancies per decile. Interestingly, that number does not appear to be evenly distributed. In deciles 1 through 9, which represent women who weigh up to 80 kg, the number of pregnancies was eight, whereas seven pregnancies occurred in the 10th decile, which represents women weighing more than 80 kg. Because the number of pregnancies in decile 10 is essentially equivalent to all of the other deciles combined, women who weigh more than 80 kg (176 lb) appear to be at increased risk of pregnancy. Five of the seven pregnancies in decile 10 occurred in women weighing more than 90 kg (198 lb).
No studies have directly explored the reasons for this relationship or looked at body mass index or body surface area in relation to efficacy of the patch. Further research is clearly needed.
How to counsel overweight women
It is imperative that patients who weigh more than 198 lb be informed that the pregnancy rate is higher than the rate quoted for the patch. It may even be reasonable to counsel women in that 10thdecile—who weigh more than 176 lb—about alternative forms of hormonal contraception that would be more effective for them than the patch.
Reference
1. Ziemen M, Guillebaud J, Weisberg E, Shangold GA, Fisher AC, Creasy GW. Contraceptive efficacy and cycle control with the Ortho Evra/Evra transdermal system: the analysis of pooled data. Fertil Steril. 2002;77(2 Suppl 2):S13-S18.
Why don’t American women choose long-acting reversible contraception?
Do American women not want to use long-acting reversible contraception (LARC), or are we, as providers, failing to properly educate them about its benefits?
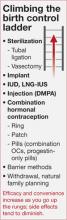
The ParaGard copper IUD, the Mirena levonorgestrel intrauterine system (LNGIUS), and the Implanon etonorgestrel contraceptive implant are all highly effective, convenient, long-duration, and reversible (FIGURE). Despite substantial evidence indicating that these methods are well tolerated and highly effective, only about 2% of American women are choosing them to prevent pregnancy.1 This rate lags far behind other countries in IUD utilization. In contrast, more than 50% of contraceptive users in China and Egypt are using intrauterine contraception.8
FIGURE
Copper IUD is effective for 12 years or longer
The copper IUD is FDA-approved for 10 years of use, although studies continue to support its continued efficacy for 12 years or longer.9 The 1-year perfect-use failure rate is 0.6%, and the typical use failure rate is 0.5% to 0.8%.10 The total failure rate over 12 years is 2.2%.9
Benefits. The copper IUD does not increase the risk of intrauterine infection and is safe to place in nulliparous patients.11 It is an excellent choice for women who clearly prefer to have monthly menses and for women who have personal or medical contraindications to hormonal birth control. Women using this method of birth control can expect excellent efficacy, rapid reversibility, and minimal side effects.
Adverse effects. The most common adverse events in copper IUD users are heavier menses and dysmenorrhea. Approximately 4.5% of women discontinue the copper IUD in the first year of use because of these particular side effects.12
LNG-IUS: Highly effective, with important noncontraceptive benefits
This method of birth control is comparable to the copper IUD in terms of efficacy and tolerability. It is FDA-approved for 5 years of use, with a cumulative 5-year failure rate of 0.7 for every 100 women.13 One small study demonstrated that this method is potentially effective up to 7 years, with a 1.1% pregnancy rate.11 With perfect use, the first-year pregnancy rate is 0.1% to 0.2%.14
Benefits. The progestin component provides noncontraceptive benefits, including a reduction in menstrual bleeding and dysmenorrhea,15 treatment of endometrial hyperplasia16 and endometrial cancer,17 endometrial protection in women using tamoxifen,18 treatment of endometriosis,19 and protection from pelvic inflammatory disease.20
Adverse effects. The primary disadvantage of this device is a change in bleeding pattern in some women, who may experience irregular spotting, primarily in the first 3 to 6 months.21 About 20% of users will become amenorrheic by 12 months of use, a feature that is highly desirable for many, but troubling to some.
Implant is essentially 100% effective
The newest LARC device is the etonorgestrel implant, which was approved by the FDA in July 2006. The single-rod implant is typically placed in the subcuticular tissue of the non-dominant arm, although placement in the dominant arm is fine if the patient prefers.