The authors report no financial relationships relevant to this article.
Over the past 10 years, the midurethral sling has replaced the Burch urethropexy as the most common surgical procedure for correcting stress urinary incontinence (SUI). In this “Update” on midurethral slings, we highlight three recently published studies that compare popular surgical approaches to SUI:
- the original tension-free vaginal tape (TVT) technique (FIGURE [“A”])
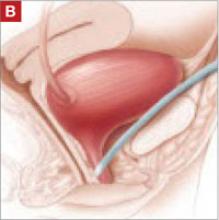
- the suprapubic urethral support sling (SPARC) (FIGURE [“B”])
- the transobturator tape (TOT) technique (FIGURE [“C”])
- the traditional pubovaginal sling (PVS), placed at the bladder neck (FIGURE [“D”]).
FIGURE [“A”] Four options for a midurethral sling to correct stress urinary incontinence: Tension-free vaginal tape (TVT) technique
FIGURE [“B”] Four options for a midurethral sling to correct stress urinary incontinence: Suprapubic urethral support sling (SPARC)
FIGURE [“C”] Four options for a midurethral sling to correct stress urinary incontinence: Transobturator tape (TOT) technique
FIGURE [“D”] Four options for a midurethral sling to correct stress urinary incontinence: Pubovaginal sling (PVS)
We’ve had a decade-plus of experience with the sling
The midurethral sling, first introduced as the tension-free vaginal tape, or TVT (Gynecare), was quick to be adopted because:
- it offers a minimally invasive approach
- it is highly efficacious
- serious adverse events are rare.
TVT utilizes a 5-mm trocar that is passed from the vagina through the retropubic space, exiting via small suprapubic incisions. A strip of permanent polypropylene mesh attached to these trocars is placed under the midportion of the urethra (FIGURE [“A”]).
We now have 11 years of follow-up data to support the use of the TVT midurethral sling for SUI.1
As TVT gained popularity, surgical equipment manufacturers developed various “kits,” so to speak, for placing a midurethral sling. Many have included innovations that have theoretical advantages over traditional TVT. Some place smaller, 3-mm trocars in a similar “bottom-up” fashion, as the TVT sling does; others utilize smaller trocars that are placed “top down” through the retropubic space into the vagina.
A later generation of slings uses the transobturator approach, to avoid blind passage of trocars through the retropubic space. These slings can be placed “in to out” or “out to in,” and rest in a slightly different orientation under the midurethra.
In an effort to make the procedure even more minimally invasive, some manufacturers now offer slings that are placed through one vaginal incision, thereby avoiding additional suprapubic or groin incisions. Other kits have made alterations to the polypropylene mesh by heat-sealing the material or applying a coating.
Such modifications haven’t always been improvements—some sling kits carried a higher incidence of mesh-related complications, and certain ones were removed from the market. And, although the number of commercially available midurethral sling kits has exploded, we’ve seen scant data published that compare the traditional TVT method with alternative approaches. Those alternatives may be considered midurethral slings, but we haven’t known whether minor variations in technique, or in the instrumentation, translate to improvements in long-term efficacy.
More readjustments for retention are needed after SPARC (vs. TVT)
Lord HE, Taylor JD, Finn JC, et al. A randomized controlled equivalence trial of short-term complications and efficacy of tension-free vaginal tape and suprapubic urethral support sling for treating stress incontinence. BJU Int. 2006;98:367–376.
This randomized, controlled trial compared TVT with SPARC to treat SUI. The study was designed as an equivalence trial: the investigators sought to determine if the “newer” intervention of the two (SPARC) is therapeutically equivalent to the existing intervention (TVT)—not whether one is superior. They therefore looked to see if patients who underwent TVT and those who underwent SPARC had the same rate (within a 5% margin) of bladder injury and other secondary outcomes.
Subjects were eligible to participate if they had SUI on the basis of urodynamic or clinical parameters. They were unaware of their assigned treatment, underwent TVT or SPARC, and were reevaluated 6 weeks postoperatively. Intraoperative, postoperative, and 6-week follow-up data were recorded by the study surgeon.
Three hundred and one patients were enrolled; 147 underwent TVT and 154 underwent SPARC. The groups were similar in regard to all baseline characteristics.