We lack data supporting placement of cerclage for an incidentally detected short cervix in women who lack a history of spontaneous preterm birth or midtrimester loss.7
Other groups known to be at increased risk of spontaneous preterm birth include women carrying twins and women who have undergone cervical cone biopsy or loop electrosurgical excision procedure (LEEP). Among twin gestations, cerclage for a short cervix is associated with an increased rate of preterm birth (<35 weeks).10 Cerclage for a short cervix has not been evaluated among women who have a history of LEEP.6
CASE RESOLVED
After preterm labor is ruled out, the patient is counseled about her options and chooses cervical cerclage. Her pregnancy proceeds uneventfully until 36 weeks’ gestation, when she delivers a healthy infant weighing 2,950 g.
When a short cervix is detected between 24 and 34 weeks
CASE 3: Is it preterm labor?
A primigravida at 31 weeks’ gestation presents to the labor floor reporting regular contractions. She denies bleeding or rupture of membranes. Contractions are noted at 3-minute intervals, and digital cervical examination reveals that she is dilated 1 cm, with 70% effacement. TVUS determines cervical length to be 17 mm.
How should she be managed?
From 24 to 34 weeks’ gestation, the prevention, diagnosis, and treatment of preterm labor become the main concerns. Because our ability to predict and prevent preterm birth is limited, clinical management focuses on a reliable diagnosis of preterm labor to allow for selective, timely interventions to optimize neonatal outcomes. These interventions include tocolysis to permit maternal transport; antibiotic prophylaxis for group B strep; and steroid administration to accelerate fetal lung maturity. Equally important is the ability to reliably rule out preterm labor among symptomatic (contracting) women to avoid the potential morbidity, cost, and inconvenience of these interventions.
Before 37 weeks, a diagnosis of preterm labor requires the following findings:
- six or more contractions per hour
- cervical dilation, as identified by digital examination, of at least 3 cm and 80% effacement.
This diagnosis is more reliable when ruptured membranes or vaginal bleeding are present.
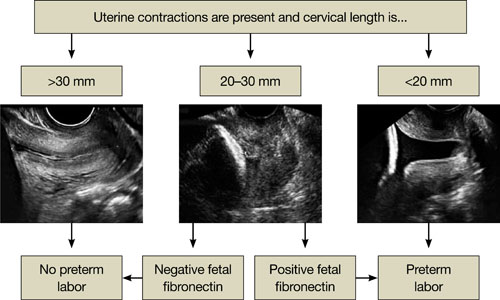
The significance of contractions without these findings is less clear. Therefore, we follow an algorithm that incorporates TVUS measurement of cervical length and evaluation of fetal fibronectin (fFN) (FIGURE 4).13
fFN is a glycoprotein that is normally confined to the extracellular matrix of the fetal membranes between 24 and 34 weeks’ gestation. Detection of fFN in cervicovaginal secretions during this window is associated with an increased risk of spontaneous preterm birth, whereas its absence demonstrates a negative predictive value for delivery within 7 days of testing of more than 97%.
During initial assessment of a regularly contracting preterm patient, perform a vaginal speculum examination. If the membranes are intact, use a vaginal swab to assess the patient for the presence of fFN, and set the specimen aside. Also obtain a culture for group B strep.
If a digital cervical examination and the contraction pattern establish a diagnosis of preterm labor, administer a tocolytic, When fetal prophylactic antibiotics, and steroids. If the diagnosis remains unclear, evaluate the cervix via TVUS. A cervical length above 30 mm effectively rules out preterm labor and obviates the need to send the fFN swab for assessment. As a result, the patient can be managed expectantly.
In contrast, a cervical length below 20 mm effectively confirms the diagnosis of preterm labor, and treatment can proceed. Again, the fFN swab may be discarded. The swab is sent for processing only if cervical length is 20 mm to 30 mm (FIGURE 4). A positive fFN result leads to the presumptive diagnosis of preterm labor, whereas a negative result permits expectant management.
We also recommend that women who display symptoms of preterm labor be screened for asymptomatic bacteriuria. Identification and treatment of this condition significantly reduce the risk of preterm delivery (RR, 0.56; 95% CI, 0.43–0.73).14 In addition, diagnosis and treatment of bacterial vaginosis in symptomatic women who have a history of spontaneous preterm birth can also reduce the risk of recurrent preterm delivery (RR, 0.42; 95% CI, 0.27–0.67).15
Not all obstetric care providers have the resources necessary for TVUS assessment of cervical length. When that is the case, fFN offers high sensitivity and negative predictive value and can help guide initial clinical decision-making. Keep in mind, however, that not all facilities offer fFN testing. In addition, in some cases, cervical manipulation may have occurred before fFN testing was performed, precluding its validity. In such cases, the incorporation of TVUS assessment of cervical length into clinical evaluation may help guide decision-making.