FIGURE 4 How to identify preterm labor at 24 to 34 weeks
CASE RESOLVED
The determination of short cervical length (17 mm) by TVUS confirms the diagnosis of preterm labor. The patient is admitted to the hospital and treated with a tocolytic, prophylactic antibiotics, and steroids. Three days later, preterm labor recurs, and she delivers an otherwise healthy infant. Future pregnancies will be managed according to the algorithm presented in FIGURE 5.
Cerclage may benefit women who have a history of spontaneous preterm birth
A recent multicenter randomized trial evaluated the efficacy of cerclage in preventing preterm birth among 302 women who had a history of spontaneous preterm birth before 34 weeks’ gestation.11 Any woman who had a cervix shorter than 25 mm between 16-0/7 and 22-6/7 weeks’ gestation was randomized to cerclage or no cerclage.
Cerclage did not significantly reduce preterm delivery before 35 weeks’ gestation, the primary outcome. Thirty-two percent of women who received cerclage and 42% of women who did not receive cerclage delivered before 35 weeks (P = .09). However, among women who had a cervix shorter than 15 mm at randomization, cerclage reduced the rate of delivery before 35 weeks by more than 75% (P = .006). Cerclage also reduced the rate of spontaneous birth before 37 weeks, compared with no cerclage (45% vs 60%; P = .01), as well as the rate of previable preterm birth before 24 weeks (6.1% vs 14%; P = .03) and the rate of perinatal death (8.8% vs 16%; P = .046).
As this study demonstrates, ultrasonographically indicated cerclage produces a number of highly clinically significant benefits in women who have a history of spontaneous preterm birth. Another important question is whether supplemental progesterone offers additional benefit beyond that conferred by cerclage in this population.
The role of progesterone in preventing preterm birth
CASE 4: History of preterm and term delivery
A woman in her third pregnancy is referred for placement of cervical cerclage, based on her obstetric history. Her first pregnancy was marked by preterm labor at 26 weeks, resulting in spontaneous preterm birth at 28 weeks. In her second pregnancy, she had cerclage placed electively at 13 weeks and delivered spontaneously at 40 weeks with no complications of pregnancy.
Is another cerclage indicated—or would progesterone be more effective?
Supplemental 17-hydroxyprogesterone caproate, given weekly in an intramuscular dosage of 250 mg, significantly reduced the rate of recurrent spontaneous preterm birth when it was administered from 16 to 36 weeks’ gestation in women carrying a singleton fetus.16 The protective effect of progesterone is most apparent in women who have a history of very preterm delivery (<32 weeks). No such benefit has been observed in twin and triplet gestations, however.17-19
Among women who do benefit from progesterone, the effect may vary. For this reason, researchers have explored the measurement of midtrimester cervical length as a means of stratifying response to progesterone.
For example, investigators randomized women who had a history of spontaneous preterm birth to daily treatment with 90 mg of vaginal progesterone gel or placebo, starting between 16 and 22-6/7 weeks and continuing until 37 weeks or delivery, whichever came first. No difference in the rate of delivery at or before 32 weeks was observed. However, a secondary analysis among progesterone-treated women who had a cervical length below 28 mm found significant declines in the rate of delivery at or before 32 weeks, admission to a NICU, and length of stay.20,21
In another trial, investigators assessed cervical length via TVUS between 20 and 25 weeks’ gestation in a general obstetric population that included women carrying twins. Women who had a cervical length below 15 mm were offered randomization to daily oral progesterone (200 mg) or placebo from 24 weeks to 33-6/7 weeks’ gestation. The rate of spontaneous preterm birth was significantly lower in the progesterone group (19% vs 34%).22
Because the ideal formulation of progesterone for the prevention of preterm birth is unknown, ACOG recommends restricting its use to women who have a documented history of spontaneous preterm birth at less than 37 weeks’ gestation.23 My practice follows the protocol of Meis and colleagues within the framework of an overall systematic algorithm (FIGURE 5).
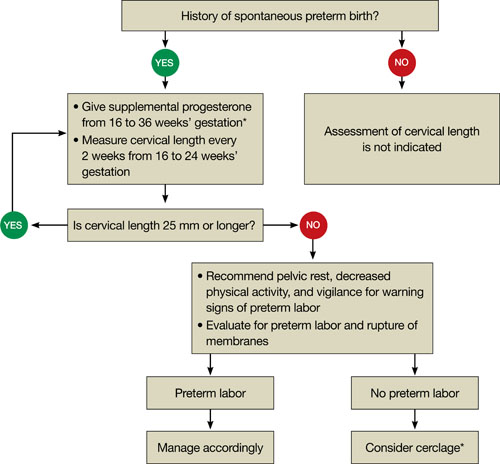
FIGURE 5 Cervical length in the second trimester
*For a singleton gestation only.
CASE RESOLVED
The ObGyn reviews the patient’s obstetric history and determines that the first pregnancy was more suggestive of preterm labor than cervical insufficiency. Therefore, the ObGyn opts for progesterone rather than cerclage to prolong the gestation. The patient begins weekly injections of 17-hydroxyprogesterone caproate, starting at 16 weeks’ gestation, with TVUS measurement of cervical length every 2 weeks. The cervix remains longer than 25 mm through 24 weeks’ gestation, at which time TVUS assessment is stopped. Progesterone injections continue through 36 weeks, and the patient spontaneously delivers a healthy 3,700-g infant at term.

