Last, researchers have long sought a simple urinary biomarker that would be specific for IC, but none are available for routine clinical use.
Although the cause of interstitial cystitis is unknown, two main theories have developed to explain it. The popular, single end-organ theory, illustrated by the pathway with red arrows in FIGURE 2, holds that an injury or insult to the bladder is the cause. When that injury fails to heal completely, the glycosaminoglycan layer of the bladder is left with a defect, allowing leakage of urinary components, such as potassium, into the mucosa and submucosa. This leakage triggers an inflammatory reaction and activates nociceptors in the bladder, including nociceptors that do not usually respond to bladder distention and stimulation (so-called silent nociceptors). Activation of these nociceptors generates allodynia in the bladder, meaning that normal distention of the bladder becomes painful.
There is evidence that other pathways also lead to IC/PBS, as illustrated by the blue, bidirectional arrows. Other generators of pelvic pain, both visceral and somatic, can neurologically activate bladder nociceptors at the central level, creating “crosstalk” and leading to bladder pain and IC/PBS. In such cases, antidromic transmission (efferent transmission in afferent nerves) can lead to neurogenic bladder inflammation and contribute further to pelvic pain. Examples of pelvic pain syndromes thought to have links to IC/PBS include endometriosis, irritable bowel syndrome, and pelvic floor tension myalgia.
In addition, there is evidence that nonpelvic syndromes, such as fibromyalgia and migraine, can lead to central or peripheral sensitization that results in IC/PBS. That is, sensitization leads to chronic bladder pain from injury or stimulation that would otherwise not cause pain.
As these theories suggest, it is likely that more than one disease and one disease pathway are encompassed within the syndrome called IC/PBS. In the opening case, it appears that a severe urinary tract infection and persistent myofascial pain, and possibly endometriosis, may have been variables leading to the development of IC/PBS.
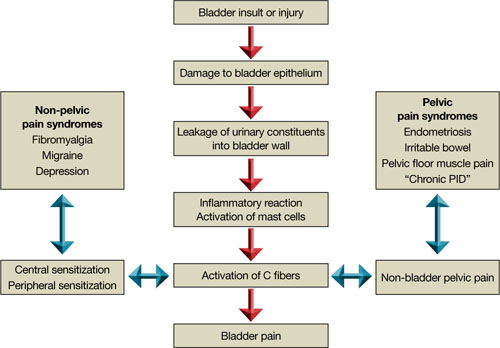
FIGURE 2 Pathways to pain
Part 2 of this article reviews components of the treatment of IC/PBS and their stepwise application.

