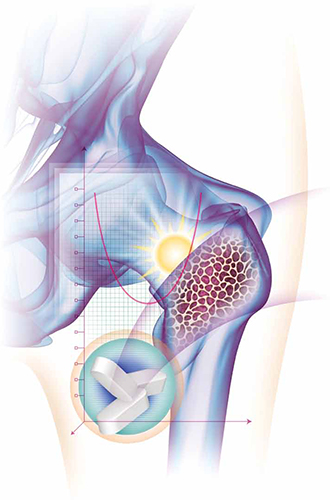
- Vitamin D plays a vital role in bone health
- The Institute of Medicine released a 2010 report that provided public health recommendations for vitamin D intake based on bone health outcomes
- Many observational studies have reported a relationship between vitamin D insufficiency and adverse nonskeletal health outcomes, including cardiovascular disease, cancer, diabetes, and autoimmune disorders, but evidence from randomized clinical trials on the potential nonskeletal benefits of vitamin D is sparse
- Excessive vitamin D intake should be avoided because of the potential for harm and the lack of evidence from well-designed clinical trials that vitamin D intake beyond the recommended amount affords greater skeletal or nonskeletal health benefits
- Among women who have an increased risk of vitamin D insufficiency or bone loss, 25OHD concentration should be measured and vitamin D supplementation should be provided as necessary to achieve the target 25OHD level
What we recommend for treatment
The IOM report provided the medical community with evidence-based recommendations for vitamin D intake at the population level, based on a public health perspective.1,2 However, the public health guideline model must be distinguished from the medical model, in which shared clinical decision-making between physician and patient occurs on an individual level and is informed by individual clinical risk factors. The public health recommendations detailed in the IOM report are not intended to replace or interfere with clinical judgment or preclude individualized clinical decision-making.
The debate over optimal levels of vitamin D supplementation for individual patients who have osteoporosis or other health conditions continues.15 Here, we provide general guidelines for treatment, based on the evidence available to date.
Clear benefits of vitamin D in bone health notwithstanding, advise your patients to avoid excessive intake because it can cause harm. See “More is not necessarily better”.
Recommendations for healthy adult nonpregnant women
Vitamin D intake: We recommend a daily vitamin D intake of 600 IU for healthy nonpregnant women up to age 70 years (and 800 Â IU daily for women older than 70 years) who are at average risk of vitamin D insufficiency and bone loss, consistent with the IOM recommendations. The IOM guidelines assume minimal to no sun exposure.
Measurement of 25OHD: It is not necessary to routinely measure the 25OHD level in these women. However, it is prudent to measure 25OHD in women who have risk factors for vitamin D insufficiency (TABLE 1) or a clinical condition associated with severe vitamin D deficiency. In these cases, if the 25OHD level is found to be below 20 ng/mL, vitamin D therapy should be initiated, with the goal of boosting the 25OHD level above the threshold of 20 ng/mL.
Treatment of vitamin D insufficiency: Options include daily vitamin D supplementation and higher-dose weekly preparations.
Many clinicians treat severe vitamin D insufficiency with 50,000 IU of vitamin D2 once weekly for 8 weeks, followed by a maintenance dose (described below) of vitamin D to preserve the target 25OHD level.5 An alternative is daily vitamin D supplementation, with the dosage based on the degree of insufficiency.
A general rule of thumb, for persons who have normal vitamin D absorption, is that every 1,000 IU of vitamin D3 ingested daily increases the 25OHD level by approximately 6 to 10 ng/mL.4,16 However, the incremental increase in the 25OHD concentration varies among individuals, depending on the baseline 25OHD level, with a greater incremental increase occurring at lower baseline 25OHD levels.
Monitoring of the 25OHD level after adjustment of the dosage is necessary to ensure that the target level is achieved.
Maintaining an adequate vitamin D level: Once vitamin D insufficiency has been corrected, a maintenance dosage of vitamin D should be selected—commonly 800 to 1,000 Â IU daily. A higher maintenance dosage may be required for persons who have genetic or ongoing environmental factors that predispose them to vitamin D insufficiency.
Vitamin D3 is reportedly more potent than D2 in increasing the 25OHD level,17 although this finding has not been universal.18 Monthly or twice-monthly administration of 50,000 IU of vitamin D2 is another option for maintenance of vitamin D sufficiency,5,16 although daily doses are more commonly used and are readily available in over-the-counter preparations.
Regardless of the regimen selected, the 25OHD level should be measured again approximately 3 months after a change in dosage to ensure that the target level has been achieved, with further dosage adjustments as indicated.
Recommendations for adult women at increased risk of skeletal disease
Measurement of 25OHD: The 25OHD level should be measured among women at increased risk of vitamin D insufficiency, bone loss, or fracture and among women who have established skeletal disease.




