CASE: Pelvic pain and a complex cyst: What now?
Your patient, a 41-year-old woman, has come to see you, reporting left lower quadrant pain. Physical examination is remarkable for fullness in the left adnexa. You order pelvic ultrasonography (US), which shows heterogeneous appearance to the left ovary (calipers), measuring 3.4 cm at its greatest dimension (see FIGURE). There is through transmission, but the lesion does not have the appearance of a physiologic cyst. Color Doppler shows no flow but there are areas that appear solid with septations.
With the full extent of the cyst unknown, what imaging study would be most helpful for you to order next?
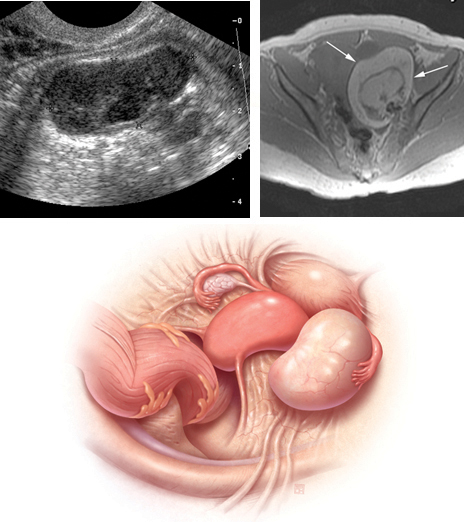
Greyscale ultrasound (top left) shows heterogeneous appearance to the left ovary (calipers), measuring 3.4 cm in greatest dimension. A T1-weighted MRI (top right) shows a 10-cm lesion (arrows) with fat. The full extent of the tumor was not recognized during the ultrasound examination.When the appearance of an adnexal lesion on US is inconclusive or nonspecific, MRI becomes a very worthwhile tool. In the case presented, MRI revealed a 10-cm fatty tumor.
I want to stress at the outset: US is always the first-line imaging tool when you assess a pelvic mass. This modality is inexpensive, widely available, and involves no exposure to radiation. In the great majority of cases in which a cyst is seen on US, it can be characterized and diagnosed appropriately and the proper treatment plan—if any is needed—established.
In women of menstrual age, most cysts that are seen on US are physiologic. If a cyst is sufficiently small and its appearance characteristic, it does not require follow-up imaging.
MRI in its appropriate role does have advantages across a range of gyn abnormalities and problems, as I describe in this article, and, therefore, appropriate indications for use in clinical problem-solving. Those advantages include:
- a detailed view of anatomy, including information gleaned from characterization of tissues
- imaging in any plane.
Skilled US imaging of the adnexal mass (4-part series)
Ilan E. Timor-Tritsch, MD and Steven R. Goldstein, MD (September-December, April 2010)
MRI isn’t of much benefit to women with breast cancer-despite a rise in its use
Janelle Yates, Senior Editor (December 2011)
Fibroids and adenomyosis
MRI is helpful for assessing the size, location, number, and type of degeneration of leiomyomata in patients in whom specific information is needed to determine the choice of therapy. MRI also can be used to distinguish between fibroids and adenomyosis— an important distinction when you are selecting appropriate therapy for bleeding, pain, and bulk-related symptoms. Adenomyomata tend to be myometrial masses with an ill-defined margin, ovoid in shape; high signal-intensity glands are seen within the myometrium on T2-weighted imaging. Fibroids, on the other hand, tend to be round and well-defined.
Prep for uterine artery embolization. Consider how MRI might be used to assess leiomyomata in a patient who is considering nonsurgical uterine artery embolization (UAE). MRI can be used to appropriately triage her, based on the likelihood of success, to hysteroscopic resection of submucosal fibroids, hysterectomy, or UAE.
Because degenerated fibroids already have lost their vascular supply, they are unlikely to respond to UAE; fibroids that exhibit preprocedure hemorrhagic degeneration, therefore, represent a relative contraindication to UAE. Such hemorrhagic degeneration is demonstrated as high signal intensity on a T1-weighted MRI scan.
MRI angiography is performed as part of preprocedure UAE, providing information on the anatomy of the uterine and ovarian arteries. This information is important: If the ovarian artery supplies the fibroids, then the procedure might not yield a good or durable result.
After UAE. Postprocedure, MRI is helpful for predicting outcome; persistent perfusion of fibroids predicts treatment failure. Outcome correlates with the degree of devascularization, not the degree of shrinkage.
MRI also can be used to assess complications of UAE, such as fibroid expulsion, endometritis, and uterine abscess. Contrast-enhanced MRI can reveal viable attachment to the uterine wall, allowing for preoperative planning when UAE has not provided a satisfactory outcome.
Complex Müllerian anomalies that cannot be fully assessed sonographically
Müllerian anomalies affect approximately 1% of all women and as many as 25% of women with infertility or who have a history of multiple spontaneous miscarriages.
In most cases, US is adequate to appropriately characterize Müllerian anomalies. Three-dimensional US in particular is helpful for assessing the fundal contour; this modality has decreased the need for MRI significantly in such cases.
When is MRI useful in this setting? MRI can be used 1) in cases in which distinguishing a septate from a bicornuate uterus will affect management and 2) when the fundal contour cannot be assessed completely sonographically. A septate uterus, for example, can be treated with hysteroscopic resection, especially if the patient has a history of more than one miscarriage; a bicornuate uterus, on the other hand, is usually not treated surgically—although such a patient needs to be followed when she is pregnant because she is at increased risk of an incompetent cervix.



