10 practical, evidence-based recommendations for perioperative antibiotic prophylaxis
Megan O. Schimpf, MD (June 2012)
Update on Menopause
Andrew M. Kaunitz, MD (May 2012)
Urinary tract infections (UTIs) are prevalent among women, afflicting as many as 60% of women during their lifetime.1 Symptoms include urgency, frequency, and dysuria. Although the diagnosis can be made on the basis of symptoms alone in many cases, urinalysis and urine cultures often are helpful in confirming it.2 The differential diagnosis includes infectious or atrophic vaginitis, urethritis from a sexually transmitted infection, urethral diverticulum, painful bladder syndrome, urinary tract calculi, and urinary tract neoplasms. Common risk factors for UTIs are listed in TABLE 1.3
TABLE 1
Risk factors for urinary tract infection in women
Premenopausal women •History of urinary tract infection (UTI) Postmenopausal women |
| SOURCE: Adapted from ACOG3 |
Recurrent UTIs are defined as three infections in 12 months or two infections in 6 months. In this Update, we explore strategies to prevent recurrent UTIs in three groups of women:
- sexually active premenopausal women
- postmenopausal women
- women undergoing pelvic surgery.
In the process, we summarize the results of five trials that explore treatment modalities such as prophylactic antibiotics, vaginal estrogen therapy, cranberry supplementation, and probiotics (TABLE 2).
TABLE 2
Summary of therapeutic strategies for prevention of recurrent urinary tract infections
| Strategy | Dose | Advantages | Disadvantages |
|---|---|---|---|
| Prophylactic antibiotics | Trimethoprim-sulfamethoxazole (Bactrim): 1 double-strength tablet* OR Nitrofurantoin: 50 or 100 mg Either drug can be given daily for 6 months or as one dose postcoitally | Highly effective Inexpensive | Potential for future microbial resistance Caution with nitrofurantoin, particularly in older patients or women who have renal insufficiency In pregnancy, nitrofurantoin is better studied |
| Vaginal estrogen** | Conjugated estrogens (0.625 mg conjugated estrogens/1 g cream [Premarin]). Give 0.5–2.0 g cream twice weekly. Estradiol (100 μg estradiol/1 g cream [Estrace]). Give 1–4 g cream | Highly effective in postmenopausal women, who can be difficult to treat Few true contraindications | Can be expensive Compliance may be an issue |
| Cranberry supplement | Dosing varies among products. Unsweetened natural cranberry juice or cranberry tablets, 1–3 times daily. | Generally well-tolerated Few side effects or contraindications | Can be expensive Compliance may be an issue May not be as effective in postmenopausal patients |
| Probiotics | Dosing varies among products and local availability | Few side effects or contraindications | Limited data Can be expensive |
| * Consider trimethoprim (100 mg) alone if the patient has an allergy to sulfa. ** Creams are preferred to the vaginal ring or tablets because they can be applied to periurethral tissues | |||
Postcoital antibiotic prophylaxis prevents some cases of recurrent UTI
Melekos MD, Asbach HW, Gerharz E, Zarakovitis IE, Weingaertner K, Naber KG. Post-intercourse versus daily ciprofloxacin prophylaxis for recurrent urinary tract infections in premenopausal women. J Urol. 1997;157(3):935–939.
UTIs typically involve fecal flora that colonize the vagina and perineum, most commonly Escherichia coli, Staphylococcus saprophyticus, Klebsiella pneumonia, and Proteus mirabilis. These pathogens ascend to the bladder via the urethra. Sexual intercourse is thought to facilitate this process, and recurrent UTIs in premenopausal women are often postcoital in temporal pattern.
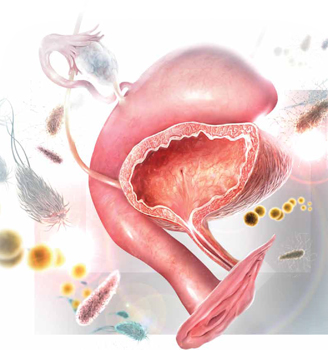
When fecal flora ascend via the urethra from the vagina and perineum to the bladder, the bladder mucosa and urethra may become inflamed, leading to urinary tract infection. The most commonly involved pathogens are Escherichia coli, Staphylococcus saprophyticus, Klebsiella pneumonia, and Proteus mirabilis.Daily antibiotic prophylaxis for 6 to 12 months has proved to be effective in the prevention of recurrent UTIs, reducing the risk of recurrence by 95%, compared with placebo.4
In this trial by Melekos and colleagues, sexually active premenopausal women who had a history of three or more documented UTIs in the preceding 12 months were randomly assigned to:
- oral ciprofloxacin, one dose daily, or
- oral ciprofloxacin, one dose immediately after intercourse.
A total of 135 patients (65 in the daily group and 70 in the postcoital group) were followed for 12 months. The regimens were equally effective at preventing UTIs. The mean number of UTIs in 12 months decreased significantly in both groups—from 3.74 to 0.031 in the daily group and from 3.67 to 0.043 in the postcoital group.
The best antibiotic? Nitrofurantoin or trimethoprim-sulfamethoxazole
This randomized, controlled trial was rigorous and well-executed and included only healthy premenopausal women. However, given the emergence of antibiotic resistance since this trial was conducted, ciprofloxacin is not an ideal antibiotic for prophylaxis.




