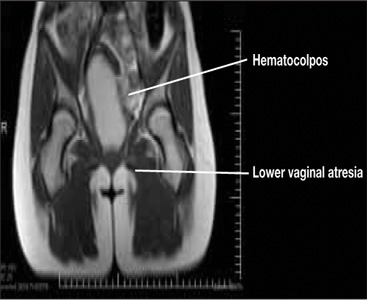
Figure 2. Lower vaginal atresia
MRI is vital to firm diagnosis
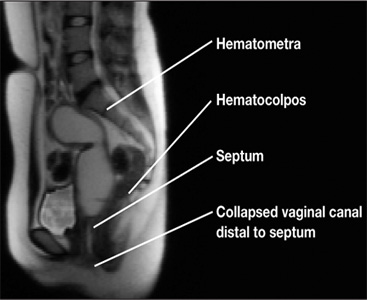
In addition to pelvic ultrasonography, pelvic MRI is necessary to delineate the anatomy with both vaginal septum (FIGURE 3) and lower vaginal atresia (FIGURE 4), as preoperative evaluation of location and thickness of a vaginal septum as well as measurement of the total length of agenesis is imperative.6-8 Misdiagnosis of the vaginal septa or atresia as an imperforate hymen can lead to significant scarring and stenosis and can make corrective surgical procedures difficult or suboptimal.
| Figure 3. MRI of transverse vaginal septum |
Figure 4. MRI of lower vaginal atresia
Surgical management: hymenectomy
Imperforate hymen is managed surgically with hymenectomy. Repair is generally reserved for the newborn period or, ideally, in adolescence, as at puberty the presence of estrogen aids in surgical repair and healing.5 Simple aspiration of hematocolpos/ mucocolpos can lead to ascending infection, and pyocolpos and should be avoided.6
The goal of hymenectomy is to:
-
open the hymeneal membrane to allow egress of fluid and menstrual flow
-
allow for tampon use
The procedure is relatively straightforward and usually is performed under general anesthesia, although regional anesthesia also is an option.
Steps to the varying hymenectomy incisions
Cruciate incision
1. Incise the hymen at the 2-, 4-, 8-, and 10-o’clock positions into four quadrants.
2. Excise the quadrants along the lateral wall of the vagina.
Elliptical incision
1. Make a circumferential incision with the Bovie electrocautery, incising the hymenal membrane close to the hymenal ring.
U-incision
1. Similar to the elliptical incision, use the Bovie electrocautery to incise the tissue close to the hymenal ring posterior and laterally in a “u” shape.
2. Make a horizontal incision superiorly to remove the extra tissue.
Vertical incision
This incision has been described in cases where there is an attempt to spare the hymen for religious or cultural preference.
1. Make a midline vertical hymenotomy less than 1 cm. Drain the borders of the hymen.
2. Apply suture obliquely to form a circular opening.
References
1. Dominguez C, Rock J, Horowitz I. Surgical conditions of the vagina and urethra. In: TeLinde’s Operative Gynecology. 10th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 1997.
2. Basaran M, Usal D, Aydemir C. Hymen sparing surgery for imperforate hymen: case reports and review of literature. J Pediatr Adolesc Gynecol. 2009;22(4):e61–e64.
Tips to a successful procedure
Ensure adequate suctioning. Before starting the procedure, insert a Foley catheter to completely drain the bladder and delineate the urethra. Making an initial incision into the hymen usually results in the expulsion of the old blood and mucus, which can be very thick and viscous; therefore, it is important to have adequate suction tubing.
Prevent scarring. After evacuating the old blood and mucus, excise the hymeneal membrane with a cruciate incision as is traditionally described. Alternatively, some experts use an elliptical incision or u-incision. (See “Steps to the varying hymenectomy incisions”.) Prevent excision of the hymenal tissue too close to the vaginal mucosa, as this can lead to scarring and stenosis and dyspareunia.3
Suturing the mucosal margins is likely unnecessary in adolescent patients. After excision of the hymenal tissue, one option is to suture the mucosal margins of the hymenal ring in an interrupted fashion with a fine, delayed-absorbable suture. Alternatively, at our institution, where we employ the u-incision (FIGURE 5), we assure hemostasis of the mucosal margins and do not suture the margins. Suturing the margins is believed to prevent adherence of the edges; however, in the pubertal girl, adherence is unlikely secondary to estrogen exposure.
Figure 5. Surgical correction with u-incision
Avoid infection; do not irrigate. We do not recommend that you irrigate the vagina and perform unnecessary uterine manipulation, as this may introduce bacteria into the dilated cervix and uterus.3,8