The use of intracytoplasmic sperm injection in fresh in vitro fertilization cycles has doubled since 1996, increasing chiefly among couples without male factor infertility, but the increase hasn’t been accompanied by any improvement in reproductive outcomes.
ICSI use in cases without male factor infertility is associated with small, but statistically significant declines in implantation, pregnancy, and live birth rates, compared with conventional IVF, Sheree L. Boulet, Dr.P.H., of the Division of Reproductive Health, Centers for Disease Control and Prevention in Atlanta, and her colleagues, reported Jan. 20 in JAMA.
The use of ICSI for men with borderline or even normal semen characteristics has increased over the past 20 years, even though there is no clear evidence of its superiority to conventional IVF. To assess national trends in ICSI use in more detail, the researchers analyzed data from the National Assisted Reproductive Technology Surveillance System for 1,395,634 fresh IVF cycles from 1996 through 2012.
Overall, about 65% of these cycles used ICSI, including 51% of cycles in which there was no male factor infertility.
The percentage of fresh IVF cycles using ICSI increased from 36.4% to 76.2% during the study period. Among couples with no male factor infertility, ICSI use increased from 15.4% to 66.9% of all fresh IVF cycles.
In the entire study population, there were no differences between cycles using ICSI and cycles using conventional IVF in reproductive outcomes. However, in the large subset of couples without male factor infertility, ICSI use was associated with significantly lower implantation rates (23.0% vs 25.2%), pregnancy rates (44.9% vs 47.9%), and live birth rates (36.5% vs 39.2%), according to the study (JAMA. 2015;313:255-63 [doi:10.1001/jama.2014.17985]).
The differences “may be a function of the large sample size and thus not clinically relevant,” the researchers wrote. But the findings suggest that the use of ICSI may improve fertilization rates, but not implementation or pregnancy rates for unexplained infertility, advanced maternal age, and low oocyte yield.
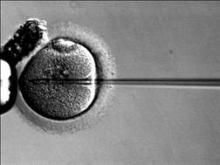
The underlying reasons for these findings are not yet known. ICSI bypasses natural barriers to fertilization, which increases the chance of fertilization, but at the same time increases the possibility of transmitting genetic defects.
It is possible that “by bypassing natural selection, ICSI use could have resulted in poorer-quality embryos, compared with conventional IVF, leading to poorer reproductive outcomes,” the researchers wrote. Another possibility is that ICSI may have been used as a rescue measure after attempts at conventional IVF failed; in such cases, oocyte quality likely was poor, leading to poorer outcomes.