Every prevention effort or treatment has its own risks. Gynecologists must consider the risk for blood clots from using estrogen-containing oral contraceptives versus the risk of blood clots from pregnancy. Endocrinologists must weigh the risk of decreased bone mineral density versus premature closure of growth plates when starting pubertal blockers for children suffering from precocious puberty. Psychologists and primary care providers must consider the risk for increased suicidal thoughts while on selective serotonin reuptake inhibitors versus the risk of completed suicide if the depression remains untreated.
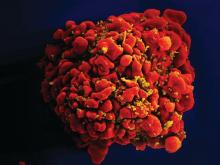
Five years ago, the Food and Drug Administration approved the combination drug emtricitabine/tenofovir (also known as Truvada) for use as pre-exposure prophylaxis (PrEP) against the human immunodeficiency virus (HIV). This profoundly changed the paradigm in HIV prevention efforts. The lesbian, gay, bisexual, and transgender (LGBT) community has largely benefited from this new approach. However, one subset of the LGBT population that has yet to benefit from PrEP is LGBT youth. Many pediatric providers are wary of the risk of using PrEP on adolescents, citing the lack of evidence of its safety and effectiveness, but a comparison of the well-known risks of HIV infection for this vulnerable population versus the little-known risk for using PrEP will provide a rationale for its use to prevent HIV among LGBT youth.In the United States alone, 22% of HIV infections occur in people aged 13-24 years. Among those with HIV infection, 81% are young men who have sex with men (MSM).1 Among those new infections, young MSM of color are nearly four times as likely to have HIV, compared with white young MSM.2 Moreover, the incidence of HIV infection among transgender individuals is three times higher than the national average.3
What further hampers public health prevention efforts is the stigma and discrimination LGBT youth face in trying to prevent HIV infections: 84% of those aged 15-24 years report recognizing stigma around HIV in the United States.4 In addition, black MSM were more likely than other MSMs to report this kind of stigma.5 And it isn’t enough that LGBT youth have to face stigma and discrimination. In fact, because of it, they often face serious financial challenges. It is estimated that 50% of homeless youth identify as LGBT, and 40% of them were forced out of their homes because of their sexual orientation or gender identity.6 Also, transgender youth have difficulty finding employment because of their gender identity.7 A combination of homelessness or chronic unemployment has driven many LGBT youth to survival sex or sex for money, which puts them at higher risk for HIV infection.7,8 The risk for HIV infection is so high that we should be using all available resources, including PrEP, to address these profound health disparities.
One of the biggest hesitations for providers to use PrEP in everyday practice is the lack of available data on its effectiveness and safety. The FDA did not approve PrEP for people under 18 years old because studies on the medications’ effectiveness and safety were conducted on people 18 years and older. The Centers for Disease Control and Prevention, however, stated that physicians should consider using PrEP for adolescents, weighing the known risks and benefits of the medication and understanding the variation in state laws regarding minors receiving treatment for prevention of a sexually transmitted disease (STD) such as HIV (some states may not consider HIV as a STD).9Studies, however, are forthcoming. One study by Hosek et al. that was published in September suggested that PrEP among adolescents can be safe and well tolerated, may not increase the rate of high-risk sexual behaviors, and may not increase the risk of other STDs such as gonorrhea and chlamydia. It must be noted, however, that incidence of HIV was fairly high – the HIV seroconversion rate was 6.4 per 100 person-years. Nevertheless, researchers found the rate of HIV seroconversion was higher among those with lower levels of Truvada in their bodies, compared with the seroconversion rate in those with higher levels of the medication. This suggests that adherence is key in using PrEP to prevent HIV infection.10 Although far from definitive, this small study provides some solid evidence that PrEP is safe and effective in preventing HIV among LGBT youth. More studies that will eventually support its effectiveness and safety are on the way.11
Use of PrEP to prevent HIV among adolescents has its risks and benefits. Providers should keep in mind that teenagers, especially LGBT youth, are at high risk for HIV; that significant barriers exist in preventing HIV in this high-risk population; and that there is growing evidence that PrEP is safe and effective at preventing HIV. Unless there is compelling evidence that would contraindicate the use of PrEP, the risk for HIV infection in LGBT youth is way too high not to consider using PrEP as part of my HIV prevention tool box, and I urge my colleagues to do the same.