While guidelines for bronchiolitis aim to reduce gratuitous tests and treatments, one-third of infants presenting at EDs with bronchiolitis receive an unnecessary intervention, according to a new global study.
For infants with symptoms of bronchiolitis, viral testing, blood tests, and chest x-rays are discouraged in most cases. Antibiotics are not recommended as treatment.
In a study published in Pediatrics, Amy Zipursky, MD, of the Hospital for Sick Children and the University of Toronto, and colleagues, reviewed records for 2,359 infants aged 2-11 months diagnosed with bronchiolitis during the year 2013. The data came from a network of 38 EDs in the Australia, Canada, Ireland, New Zealand, Portugal, Spain, the United Kingdom, and the United States.
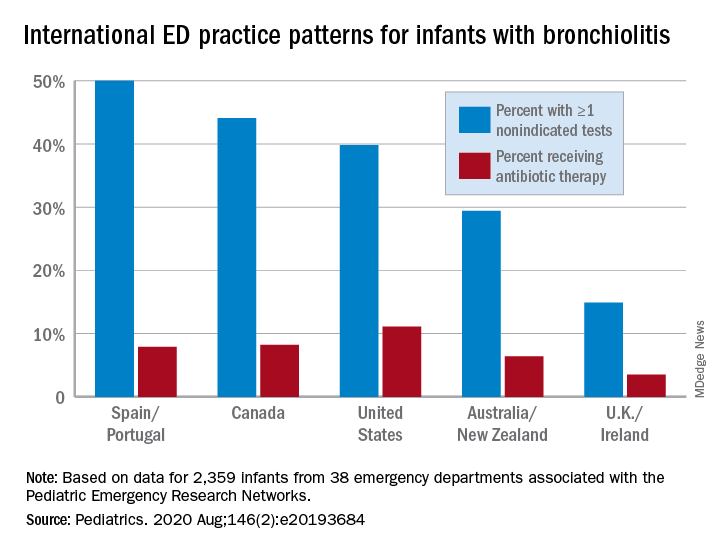
Dr. Zipursky and colleagues found that, while 8% of infants in the cohort had been treated with antibiotics, 33% had received at least one nonrecommended test, with rates ranging widely across regions. In the United Kingdom and Ireland, for example, only 15% received such a test, compared with 50% in Spain and Portugal.
Of the children given antibiotics, two-thirds had suspected bacterial infections, the researchers found. Antibiotic use was highest in the United States, at 11% of infants seen for bronchiolitis, and lowest in the United Kingdom and Ireland at 4%. Administration of chest x-rays – which occurred in nearly a quarter of the cohort – increased the likelihood of antibiotics being administered (odds ratio, 2.29; 95% confidence interval, 1.62-3.24) independent of fever or severe symptoms.
The most common nonrecommended tests performed in the study were:
- Nasopharyngeal viral testing without admission to hospital (n = 591).
- Chest x-ray without ICU admission (n = 507).
- Complete blood counts (n = 222).
- Blood cultures (n = 129).
- Urinalysis in the absence of fever (n = 86).
- Febrile infants 3 months of age or less had blood cultures (n = 49).
In some treatment centers the rate of nonrecommended tests performed was 6%, while others saw rates of 74%.
“Despite the evidence that laboratory testing rarely impacts bronchiolitis management and that bacterial infections in bronchiolitis are uncommon, our study reveals that these tests continue to be performed frequently in many parts of the world,” Dr. Zipursky and colleagues wrote in their analysis.
“Plausible reasons may include ‘automatic’ blood draws with intravenous placement, uncertainty about institutional policies, perceived need for reassurance about the diagnosis, perception of ‘doing something,’ and parental desire for a viral label,” the authors surmised. “Because parental pressure to provide interventions may be a driver of care in infants with bronchiolitis in some countries, ED clinicians need to have higher confidence in the evidence-based bronchiolitis care and convey this trust to families.”
The researchers listed among the weaknesses of their study its retrospective design, and that results from x-rays and lab tests performed were not available.
In an editorial comment accompanying the study, Joseph J. Zorc, MD, of Children’s Hospital of Philadelphia and the University of Pennsylvania in Philadelphia, noted that some of the regional differences seen in the study may be attributable to different clinical criteria used to diagnose bronchiolitis. In the United Kingdom, for example, national guidelines include the presence of crackles, while in North America guidelines focus on wheeze. “Perhaps clinicians in the United Kingdom accept the presence of crackles as an expected finding in infant with bronchiolitis and are less likely to order imaging,” Dr. Zorc said (Pediatrics. 2020 Jul 13;146[2]:e20193684).
He also pointed out that the coronavirus pandemic caused by SARS-CoV-2 (COVID- 19) could have an impact on global testing and treatment practices for bronchiolitis, as coronaviruses are a known cause of bronchiolitis. The Pediatric Emergency Research Network, comprising the 38 EDs from which Dr. Zipursky and colleagues drew their data, is conducting a prospective study looking at pediatric disease caused by SARS-CoV-2.
The “collaboration of international networks of pediatric emergency providers is an encouraging sign of potential opportunities to come ... [providing] an opportunity to evaluate variation that can lead to innovation,” Dr. Zorc concluded.
Dr. Zipursky and colleagues reported no external funding or relevant financial disclosures. Dr. Zorc reported no relevant conflicts of interest.
SOURCE: Zipursky A et al. Pediatrics. 2020 Jul 13;146(2):e2020002311.