Artemisinin-resistant Plasmodium falciparum malaria remains uncontained. It is now "firmly established" in western Cambodia and Thailand, southern Vietnam, and eastern Myanmar and is emerging in southern Laos and northeastern Cambodia, according to a report published online July 31 in the New England Journal of Medicine.
"Radical measures will be necessary in Southeast Asia to prevent resistance to artemisinins and their partner drugs from spreading to the Indian subcontinent and then to Africa," said Dr. Elizabeth A. Ashley of the Mahidol-Oxford Tropical Medicine Research Unit, affiliated with both Mahidol University in Bangkok, Thailand, and the University of Oxford (England), and her associates.
Artemisinin resistance was first reported in western Cambodia in 2008, and that is where resistance to previous first-line antimalarials also first emerged. "Defining the extent and severity of artemisinin resistance is essential for planning containment and elimination strategies," the investigators noted.
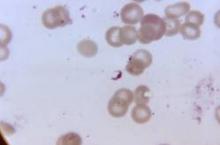
To map the current extent of artemisinin resistance, they performed an open-label, randomized trial at 15 sites in Cambodia, Thailand, Laos, Vietnam, Myanmar, Bangladesh, India, Nigeria, Kenya, and the Congo. Over a 2-year period, 1,241 patients aged 6 months to 65 years with acute, uncomplicated falciparum malaria were randomly assigned to receive either 2 mg or 4 mg of oral artesunate for 3 days, followed by a standard 3-day course of artemisinin-based combination therapy. Parasite clearance half-life was then determined using serial blood smears. Longer parasite clearance half-life is associated with the organism’s increasing resistance to the drug.
Parasite clearance half-life varied widely across the sites in Southeast Asia, from a low of 2 hours in Laos to a high of 7 hours in Thailand. Slowly clearing infections, which were defined as a parasite clearance half-life of 5 hours or longer and indicated established resistance, were detected throughout mainland Southeast Asia, but they were not yet common in India or Africa. Another measure of artemisinin resistance – the proportion of patients with parasitemia detectable on day 3 – ranged from 0% in Kenya to 68% in eastern Thailand (N. Engl. J. Med. 2014 July 31 [doi: 10.1056/NEJMoa1314981]).
However, "despite the recent spread of resistance, we found that artemisinin-based combination therapies ... were still highly efficacious, presumably because of increased reliance on the efficacy of the partner drug as the potency of the artemisinin component waned," Dr. Ashley and her associates said.
Nevertheless, they cautioned that treatment failure rates for artesunate plus mefloquine (in Thailand) and for dihydroartemisinin plus piperaquine (in Cambodia) have risen by a factor of 5.
This study was supported by the U.K. Department for International Development, the Worldwide Antimalarial Resistance Network, the U.S. National Institute of Allergy and Infectious Diseases, and the Bill & Melinda Gates Foundation. Dr. Ashley and her associates reported no relevant conflicts of interest.