Continued care for RA
This component of the payment structure also can be made to a rheumatologist, a nurse practitioner or physician assistant under the supervision of a rheumatologist, or the rheumatologist–primary care physician team. Continued care payments are made monthly and, just as with initial treatment payments, they are meant to replace E&M billing for office visits and pay for the same kinds of resources used in initial treatment, including stratified payments to adjust for patient characteristics.
Patients who come to a rheumatologist with established RA would enter this treatment pathway under this kind of payment.
RA APM’s accountability requirements
Participants in this model would be required to see a patient face-to-face at least every 6 months and to document their disease activity using a validated scale approved by the ACR for use in the RA APM, such as the RAPID-3 (Routine Assessment of Patient Index Data–3), the CDAI (Clinical Disease Activity Index), the SDAI (Simple Disease Activity Index), or the DAS28 (28-joint Disease Activity Score). Payment would also require keeping a written treatment plan that’s consistent with the ACR’s approved treatment pathway.
Changes in medication require communication with the patient within 2 weeks to help improve treatment adherence. Quality measures will still need to be recorded, such as a functional assessment, tuberculosis screening prior to starting biologics, and having a plan for steroid use, but they are not required to be reported. “You attest to that,” he said.
However, participants will need to report that they are following the treatment pathway for patients and an outcome measure for continued care of RA. These are necessary, Dr. Huston said, because “we are asking that we increase the money that’s going to the rheumatologist for managing patients with RA, so we have to show that we’re accountable and doing good with that money and that we’re taking care of our patients. ... and if we have an outcome measure, then we don’t have to report all those process measures that we do in MIPS.”
The outcome measure would be reporting:
• At least (some %) of patients with low disease activity remained in low disease activity.
• At least (some %) of patients with moderate disease activity stayed in the same or a lower disease activity category.
• At least (some %) of patients with a high disease activity had a lower disease activity category.
It’s unknown yet what the threshold percentage for each disease activity level would be, but it will be obtained from the ACR’s Rheumatology Informatics System for Effectiveness (RISE) Registry and will be refined over time from there. The outcome measure is not validated yet – none exists for RA for use in clinical practice – because it’s not yet known how to risk stratify patients in these disease activity levels for their comorbidities and socioeconomic factors. “Those are all things we need to learn over time,” Dr. Huston said, “but this is our good-faith effort at developing an outcome measure which we think will become more robust as we gather more and more data.”
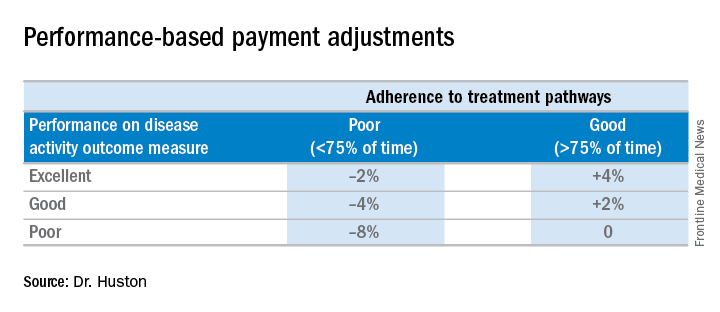
Since the outcome measure is not validated, there would be no penalty for poor performance on it. The only penalty that can be incurred in the model is if the treatment pathway is not followed at least 75% of the time.Performing all of these requirements would likely require more staff, and so the model will be built to account for these higher costs, Dr. Huston said.
Advantages of the RA APM
The RA APM’s advantages, according to Dr. Huston, stem from its payment for high-value services; the avoidance of the penalties and reporting burdens imposed by MIPS; a reduction in documentation requirements, allowing clinicians to take notes on history of present illness and review of systems however they want; a reduction in prior authorizations; and more control over performance measures.
Another big advantage of the RA APM is that participants “are not responsible for the price of drugs, whereas in MIPS you are responsible. When [the Centers for Medicare & Medicaid Services] calculates your cost category [in MIPS], that includes Part B drugs, and when the MIPS adjustment factor is applied to your revenue, that includes revenue from Part B drugs,” Dr. Huston said.
In addition, he noted that it will be possible for a rheumatologist to be a participant in just one or two APMs and still have the benefit of being out of MIPS.
Next steps
The next steps for the development of the RA APM include refining the treatment pathway, analyzing RISE data outcome thresholds, and modeling the financial impact on practices by running data from three to five practices across the country through the model to determine what the payment levels should be. Once those steps are completed, the RA APM can be submitted to the Physician-Focused Payment Model Technical Advisory Committee for approval, which will then send it to the CMS to run it through its Innovation Center to test the model in several practices to gather more data and refine the payment rates until it is ready to be expanded and implemented.