A light-cured hydrogel combined with microfracture encouraged cartilage repair in knee joints and was associated with reduced pain, a small pilot trial has found.
When applied to a debrided defect in a knee joint, the gel seeped into subchondral microfracture, trapping blood released by microfracture and forming a clot that filled most of the bone defect. Compared with clots formed solely by microfracture, the gel-clot was larger in volume, suggesting that it "may be able to retain more proteins and cells in the defect space ... further augmenting the biological factors that can promote new tissue growth," Blanka Sharma, Ph.D., of Johns Hopkins University, Baltimore, and her colleagues wrote Jan. 9 in Science Translational Medicine.
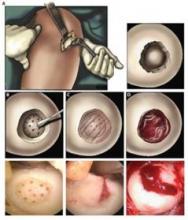 Courtesy of Science Translational Medicine/AAAS
Courtesy of Science Translational Medicine/AAAS
Clinical procedure for adhesive-hydrogel implantation into a cartilage defect. Both schematics and actual patient images are shown for the final steps. (A) A mini-incision approach was created to expose the cartilage defect. The defect edges were debrided to remove any dead tissue at the cartilage edge. (B) The adhesive was then applied to the base and walls of the defect followed by surgical microfracture. (C) Last, the hydrogel solution was injected into the defect and photopolymerized in situ with light. (D) Bleeding from the microfracture holes was trapped in and around the hydrogel.
The authors employed the light-polymerized gel with microfracture in 15 patients with a 2-4 cm2 symptomatic cartilage defect on the medial femoral condyle; three patients with similar defects underwent standard microfracture surgery. The study compared healing, function, and pain over a 6-month postoperative period (Sci. Trans. Med. 2013;5:167ra6).
At 3 months after surgery, MRI scanning in the investigational group showed a combination of clot material, hydrogel, and synovial fluid in the defect. By 6 months, new tissue filled an average of 86% of the defect in the investigational group, compared with an average defect fill of 64% in the microfracture-only group – a significant difference.
Most patients in the investigational group evaluated by MRI (12 of 14) had more than a 75% defect filling, compared with 1 of the 3 control patients.
Most patients who received the hydrogel also experienced significant reductions in pain frequency and severity, with the biggest improvements occurring in the first 3 months after surgery. One patient in this group continued to have pain at 6 months. The probable cause of pain was a misalignment in the treated knee, since the defect was more than 75% filled with new tissue, the authors said.
Control patients experienced similar significant reductions in pain frequency and severity during the first 3 months after surgery. By 6 months, one patient in the group continued to experience improvements in pain; this person "also had a high defect fill (84%), whereas the other two patients had fill values less than 75%," the authors noted.
At 6 months, pain frequency scores were not significantly different between the two groups. There were similar findings in pain severity scores. Knee function improved similarly in both groups.
The study was funded by the National Institutes of Health and the Arthritis Foundation. None of the authors had any financial disclosures.

