Case 2
An 11-year-old boy with no significant medical or surgical history fell onto his right dominant upper extremity while doing a jump on his dirt bike 1 week prior to presentation, sustaining a clavicle fracture. This was an isolated injury. He was seen and evaluated by an outside orthopedist who noted that the soft-tissue envelope was intact and the patient was neurovascularly intact. Radiographs showed a displaced fracture of the midshaft of the clavicle with 15% shortening and with a vertically angulated piece of comminution (Figure 1C). Nonoperative treatment with a figure-of-8 brace was recommended. The patient’s discomfort completely resolved.
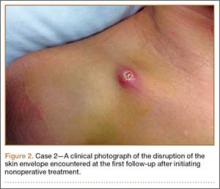
One week later, when he presented to the outside orthopedist for follow-up, the development of a wound overlying the fracture site was noted, and the patient was started on oral trimethoprim/sulfamethoxazole and referred to our office for treatment (Figure 1D). The patient denied reinjury and endorsed compliance with brace immobilization. On examination, the patient was afebrile and was noted to have a puncture wound at the fracture site with a protruding spike of bone and surrounding erythema but without present or expressible discharge (Figure 2). The patient was taken urgently for I&D and ORIF, using a similar technique to case 1, except that no lag screw was employed.
Postoperatively, the patient did well with no complications; he was prescribed oral cephalexin for 1 week. The patient was immobilized in a sling for the first 5 weeks after surgery until radiographic union had occurred, after which the sling was discontinued. The patient’s wound healed uneventfully and with acceptable cosmesis. The patient was released from activity restrictions at 6 weeks postoperatively. At final follow-up 5 weeks after surgery, the patient had full painless range of motion, no tenderness at the fracture site, no signs of infection on examination, and radiographic union (Figure 1D).
Discussion
Optimal treatment of displaced clavicle fractures is controversial. While nonoperative treatment has been recommended,1-3 especially in skeletally immature populations with a capacity for remodeling,7-9 2 recent randomized clinical trials have demonstrated improved patient outcomes with ORIF.6,8,9 Traditionally, ORIF was recommended with tenting of the skin because of concern for an impending open fracture. However, recent review materials have implied that this complication may only be theoretical.3,5 Indeed, in 2 randomized trials, sufficient displacement to cause concern for impending violation of the skin envelope was not listed as an exclusion criteria.8,9 We report 2 cases of displaced comminuted clavicle fractures that were initially managed nonoperatively but developed open lesions at the fracture site. This complication, while rare, is possible, and surgeons must consider it as a possibility when assessing patients with displaced clavicle fractures. To the best of the authors’ knowledge, no guidelines exist to direct antibiotic choice and duration in secondarily open fractures.
These 2 cases have several features in common that may serve as risk factors for impending violation of the skin envelope. Both fractures had a vertically angulated segmental piece of comminution with a sharp spike. This feature has been identified as a potential risk factor for subsequent development of an open fracture in a case report of fragment excision without reduction or fixation to allow rapid return to play in a professional jockey.13 Both patients in these cases presented with high-velocity mechanisms of injury and significant displacement, both of which may serve as risk factors. In the only similar case the authors could identify, Strauss and colleagues14 described a distal clavicle fracture with significant displacement and with secondary ulceration of the skin complicated by infection presenting with purulent discharge, cultured positive for methicillin-sensitive Staphylococcus aureus, requiring management with an external fixator and 6 weeks of intravenous antibiotics. Because both cases presented here occurred in healthy adolescent patients who were taken urgently for I&D and ORIF as soon as the wound was discovered, deep infection was avoided in these cases. Finally, in 1 case, a figure-of-8 brace was employed, which may also have placed pressure on the skin overlying the fracture and may have predisposed this patient to this complication.
Conclusion
In displaced midshaft clavicle fractures, tenting of the skin sufficient to cause subsequent violation of the soft-tissue envelope is possible and is more than a theoretical risk. At-risk patients, ie, those with a vertically angulated sharp fragment of comminution, should be counseled appropriately and observed closely or considered for primary ORIF.