If you pay a medical malpractice claim once, chances are you’ll pay a second claim in the future, according to a study published Jan. 28 in the New England Journal of Medicine (doi: 10.1056/NEJMsa1506137).
David M. Studdert Sc.D., of Stanford (Calif.) University and his colleagues analyzed 66,426 malpractice claims from the National Practitioner Data Bank that were paid against 54,099 physicians between 2005 through 2014. Investigators calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians.
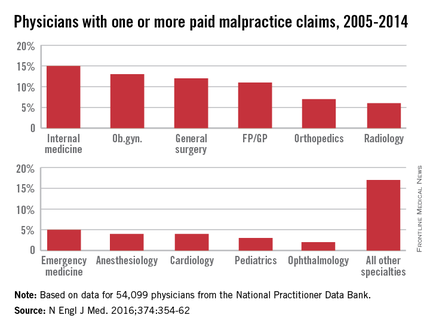
Of all paid claims, 82% involved male physicians. The specialists with the most paid claims were internists (15%), ob.gyns. (13%), general surgeons (12%), and family physicians (11%). Only 3% of the lawsuits were paid through trial verdicts. The remaining claims were paid by out-of-court settlements. The mean payment amount for claims was $371,054, while the median was $204,750.
When using all 915,564 active U.S. physicians as a denominator, only 6% of physicians had a paid claim against them and about 1% had at least two paid claims against them. When looking at physicians with at least one paid claim, 84% had only one paid claim over the study period, accounting for 68% of all paid claims. However, 16% (8,846 physicians) had at least two paid claims, accounting for 32% of all claims. A total of 4% of doctors (2,160 physicians) had at least three paid claims and accounted for 12% of all claims, and 1% (722 physicians) had at least four paid claims and accounted for 5% of all claims.
Specialties had a marked impact on the risk of future paid claims. Compared with internists, the risk of recurrence was double among neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, and ob.gyns. Psychiatrists and pediatricians had the lowest risks of recurrence.
Mr. Studdert said that the investigators were surprised to learn the degree to which past paid claims predicted future claims.
“I think if you ask most people who work in the liability insurance industry, they would tell you that’s probably true,” he said in an interview. “But I don’ t think we’ve seen – at least not on this scale – research finding just how sharply claim risk rises with malpractice history. It does suggest for those multiclaim physicians, that there is something going on that is predisposing them to be the subject of malpractice litigation.”
He noted the analysis suggests that it is feasible to predict which physicians are at higher risk for future claims. The information could then be used to develop interventions to address malpractice claims.
“These multiclaim physicians do appear to have some distinctive characteristics, and that gives us some optimism that it might be possible to predict who is going to [become] a multiclaim physician,” Mr. Studdert said. “More work is needed to make sure that’s technically feasible, but if it is, that opens up a lot of possibilities for liability insurers, hospitals ,medical boards, and other regulators to use this information proactively rather than just reacting to events after they happen.”
On Twitter @legal_med