As the United States becomes increasingly diverse, with predictions that by 2045 minorities will comprise 50% or more of the population,1 the demographics of the orthopedic surgery population will also likely diversify. It is important that orthopedic surgeons shift in their diversity as well. Lack of diversity in orthopedics (women and racial minorities are underrepresented) relative to the national population and other surgical specialties and their training programs is well documented.2-8
More concerning, the diversity of orthopedic residents does not compare favorably with that of medical school attendees.4,9 The difference suggests the greatest loss of potential diversity occurs during the transition from medical school to residency. A national study demonstrated that instruction in musculoskeletal medicine led to an increase in application rates nationally.10 However, the authors of that study stated they were unexpectedly limited by its large size—they could not validate the accuracy of curriculum data and could not differentiate between a 1-day required experience and a 4-week rotation.
In the present study, which accounted for curricular factors, we compared our medical students’ application rates to orthopedics residencies based on sex and race before and after introduction of a required third-year musculoskeletal clerkship. We hypothesized that making the curriculum a requirement would increase the number of applicants and increase the diversity of applicants in terms of both women and underrepresented minorities. This hypothesis was based on the rationale that these groups might not consider an orthopedics residency without first being directly exposed to orthopedics. We also wanted to determine what factors influenced applicants to choose orthopedic surgery.
Methods
Curriculum
Before 2006, third-year students spent 3 months completing a surgery clerkship. Some students interested in orthopedic surgery would have to wait until their fourth year to complete an elective in orthopedic surgery, and uninterested students would not be exposed at all. Starting in 2006, 1 month of the third-year surgery clerkship was required to be completed in musculoskeletal surgery: orthopedic surgery, plastic surgery, or neurosurgical spine. Plastic surgery was an option, as it exposed students to hand surgery and flap reconstruction.
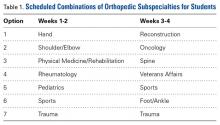
The orthopedic surgery curriculum included two 2-week experiences with an orthopedic surgeon (Table 1), twice-weekly lectures by orthopedics faculty, weekly physical examination sessions, and 3 or 4 nights of call.During the 12-year study period, overall teaching hours in the preclinical curriculum did not change, and there were no other structural changes to the preclinical or clinical curriculum. The orthopedics department increased its faculty from 23 in 2000 to 34 in 2012. Number of female faculty increased from 1 to 3, representing a 4% to 9% increase in department faculty. Throughout the 12 years, there were no underrepresented minority faculty. Total number of residents increased from 26 in 2000 to 30 in 2012. Number of female residents varied year to year, from a low of 3 in the period 2003–2004 to a high of 11 in the period 2009–2010. Number of underrepresented minority residents varied yearly as well, from 1 to 2.
Data Collection
After this study was granted exempt status by our Institutional Review Board, we obtained student data from our registrar. Data included graduation year, self-identified sex and race, exposure to orthopedic surgery during clerkships, and matching residency specialty. National data were obtained from the Electronic Residency Application Service for the periods 2002–2007 and 2009–2012. These data included all US allopathic medical students’ self-identified sex and race, and applied-to primary residency specialty. National data from 2008 and national data on sex differences in orthopedic applications from 2009 were not available.
Graduates who matched into orthopedic surgery were asked to complete an anonymous survey on what influenced their decision to apply to orthopedic surgery and when this decision was made. Our goal with the survey was to substantiate or refute the conclusion that application rates depended on third-year exposure to musculoskeletal medicine.
Statistical Methods
Students were divided into 2 groups: precurriculum (graduated within 7-year period, 2000–2006) and postcurriculum (graduated within 6-year period, 2007–2012). A 2-sample test for proportions was used to compare percentage of total students who applied to orthopedics in each group. In the group of students who applied to orthopedics, we compared precurriculum and postcurriculum proportions of women and underrepresented minorities (non-white, non-Asian). We also compared these proportions with national data (using 2-sample tests for proportions) to determine if any change in diversity of our institution’s applicants was mirroring a national trend. Our definition of underrepresented minority was based on work that showed that the proportion of Asian matriculants in medical school and the proportion of applicants to orthopedics are higher than their respective national proportions.5 Survey data are reported descriptively. Statistical significance was defined with a 2-tailed α of 0.05 for all tests.