Take-Home Points
- The location of a bicortical defect in proximity to a tibia plate does not appear to affect the torsional stiffness or torsional failure strength of the bone.
- External fixator pin placement should be based on considerations other than the potential for creating a distal stress riser after definitive fracture management.
A stress riser in cortical bone may be considered any abrupt change in the contour or consistency of the hollow structure, such as a surface defect, that not only weakens the bone but concentrates stresses at that transition point.1 A cortical defect that is 20% of the bone diameter is associated with a 34% decrease in torsional strength, thus representing a “stress riser.”2 High-energy and complex tibia fractures are often provisionally stabilized with external fixation that gives the soft tissues time to recover before definitive fracture fixation. Pin diameter for a medium-size tibia external fixator typically is 5.0 mm, resulting in a 10-mm defect in bicortical placement. Therefore, any tibia with a diameter of <50 mm is at risk for a stress riser fracture.
Although it had been established that sizable cortical defects can decrease the torsional strength of long bone,2 the effect of a plate in close proximity to a defect secondary to an empty external-fixator pin site on torsional strength has not been determined. We conducted a study to evaluate this effect. The null hypothesis was there would be no difference in tibia torsional strength attributable to varying the proximity of a tibia midshaft plate to a 5.0-mm bicortical defect.
Methods
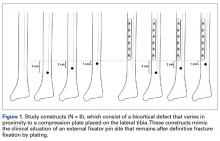
Forty fourth-generation, medium-size left composite tibias (Pacific Research Laboratories) were divided into 8 groups of 5 bones (Figure 1).
To represent the stress riser created by the removal of a 5.0-mm Schantz external fixation pin, we produced distal tibia bicortical defects in 6 of the groups by creating anterior-to-posterior 5.0-mm bicortical drill holes. The longitudinal location of these drill holes was varied in relation to the distal end of a 4.5-mm × 121-mm 6-hole locking plate (PeriLoc; Smith & Nephew) fixed in a nonlocking configuration and positioned across the tibia midline on the anterior-medial aspect. In the experimental plated groups, the bicortical defects were created 3.0, 2.0, and 1.0 cm distal to the plate end, with 1 plated group without a defect. The control groups consisted of equivalent defects in the same distal longitudinal locations, without plates attached, as well as an unplated group without a defect.Torsion testing to failure was performed for all specimens in a manner similar to that described by Gardner and colleagues.3 Impression molds for the composite tibia constructed from polymethylmethacrylate encased the superior and distal ends, leaving 25.5 cm of exposed midshaft. This allowed the composites to be rigidly clamped into a materials testing system (858 Mini-Bionix; MTS) equipped with a 100.0-Nm torsional load cell (Figure 2).
The constructs were preconditioned by rotating the superior end internally up to 15.0 Nm at a rate of 0.25 Nm/s for 2 complete cycles. Next, the constructs were preloaded axially to 20.0 N and then rotated at 0.25°/s until failure. Torsional load and torsional displacement were recorded and used to determine construct stiffness and failure load. Stiffness was calculated as the slope of the linear elastic portion of the load versus displacement curves between 20.0 Nm and 40.0 Nm. Failure load was defined as the highest load achieved before fracture. One-way analysis of variance with Tukey adjustment for multiple comparisons and α set at 0.05 were used to detect differences in failure stiffness and failure load between the 8 constructs.Results
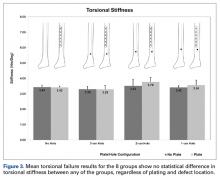
Graphical results for torsional stiffness are presented in Figure 3. R2 for all stiffness calculations was >0.99.
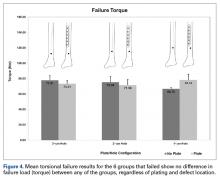
There were no statistical differences in torsional stiffness between any of the groups. Graphical results for torsional failure load are presented in Figure 4. During torsion-to-failure testing, both plated and unplated specimens without distal cortical defect holes nearly exceeded the torque capacity of the load cell without failing, stopping the tests. For the specimens that failed, there were no statistical differences in failure torque. A slight trend toward higher failure loads in plated specimens with a hole in close proximity was seen in the 1.0-cm distal defect hole groups, with the plated specimen achieving a higher mean (SD) failure load, 78.14 (7.58) Nm, than the unplated group, 66.75 (1.84) Nm, but this was not significant (P = .06). Another slight trend toward lower failure load in unplated specimens as the defect moved proximally was seen between the unplated 3.0-cm defect group, 77.91 (6.08) Nm, and the unplated 1.0-cm defect group, 66.75 (1.84) Nm; this was also not significant (P = .07). Mode of failure for all specimens with bicortical defects, with or without a plate, was a spiral fracture that bisected the axis of the defect (Figure 5). Post hoc power analysis for each measure indicated statistical power of 80% for stiffness and 75% for failure torque.