Adherence to guidelines for urinary catheter removal significantly reduced rates of urinary tract infection and length of hospital stay, based on data from almost 3,000 patients.
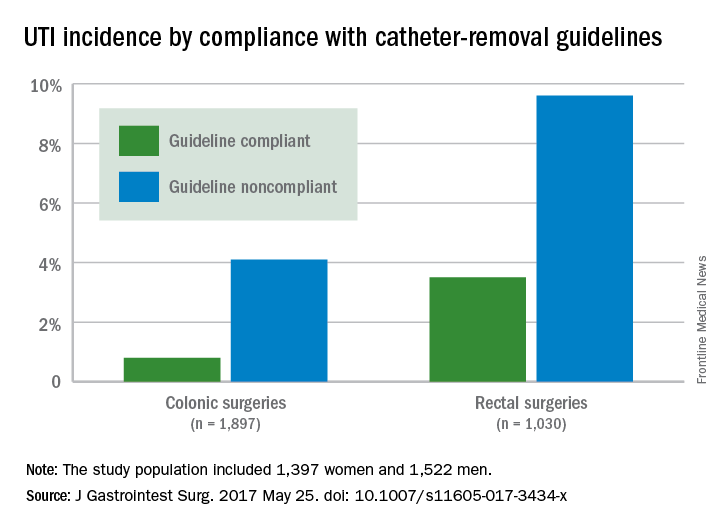
UTIs occurred in 0.8% of colonic surgery patients who were guideline compliant, compared with 4.1% of noncompliant patients. Similarly, UTIs were significantly less likely in rectal surgery patients who complied with guidelines, compared with those who did not (3.5% vs. 9.6%).
The Implementation of the Enhanced Recovery After Surgery (iERAS) program involved 15 academic hospitals in Ontario, Canada. The guidelines include prompt removal of catheters from colonic and rectal surgery patients. Recommended removal times ranged from 24 hours to 72 hours, depending on the procedure.
“Although numerous reports have documented the overall effectiveness of bundled ERAS interventions improving outcome, the contribution of individual components of the pathway in the context of an ERAS implementation program is uncertain,” wrote Allan Okrainec, MD, of the University of Toronto, and his colleagues.
To assess the guidelines’ impact on urinary tract infections and hospital stay, the researchers collected data from 2,927 surguries in adults, including 1,897 colonic or small bowel procedures and 1,030 rectal procedures, between September 2012 and April 2015. The study population included 1,397 women and 1,522 men, with an average age of 60 years (J Gastrointest Surg. 2017 May 25. doi: 10.1007/s11605-017-3434-x).Overall, 53% of patients had catheters removed in compliance with the guidelines, including 47.2% of those with colonic resections and 69.5% of those with rectal resections.
The average length of hospital stay for colonic surgery patients who complied with the urinary catheter guideline was 4 days, compared with 5 days for noncompliant patients, a statistically significant difference. Similarly, the average length of stay was significantly shorter for compliant rectal surgery patients, compared with noncompliant patients (5 days vs. 8 days, respectively).
Reinsertion of the urinary catheter was needed for 6% of the patients, including 122 patients with suspected or confirmed urinary retention and 36 patients who had other indications for reinsertion.
“One of the concerns about early removal of catheters is that it might lead to an increased need for reinsertion,” the researchers noted. “In our study, guideline compliance was associated with an increased rate of catheter reinsertion, but [it] only increased the risk by 2%-3% in patients having rectal or colonic procedures,” the investigators said.
The study results were limited by a lack of information about reasons for noncompliance with the guidelines, the researchers added. However, the data support the value of early catheter removal for surgical patients. “It is noteworthy that, in our study, as well as others, urinary retention rates are relatively low,” they said.
The Council of Academic Hospitals of Ontario funded the study. The researchers had no financial conflicts to disclose.