Diagnosis
There have been 8 histologic and clinical criteria described to diagnose Gorham disease: (1) biopsy positive for presence of angiomatous tissue, (2) complete absence of any cellular atypia, (3) lack of osteoclastic response and lack of dystrophic calcifications, (4) evidence of progressive resorption of native bone, (5) no evidence of expansive or ulcerative lesion, (6) lack of visceral involvement, (7) osteolytic radiographic pattern, and (8) no concrete diagnosis after hereditary, metabolic, neoplastic, immunologic, and infectious work-up.4-6 These criteria confirm that the diagnosis can be rendered only after exclusion of neoplastic and infectious etiologies through clinical and laboratory work-up, imaging studies, and tissue sampling.
Tissue biopsy is indicated to rule out other potential etiologies of osteolysis, and the histologic findings help confirm a diagnosis of Gorham disease.
Biopsies typically show a progressive osteolysis that is consistently associated with a benign but abnormal vascular proliferation that in many cases has characteristics of lymphatic endothelium. The apparent bony destruction is largely attributed to this process (Figures 5A-5D).11,12The differential diagnosis includes infection (osteomyelitis, Brodie abscess), benign tumors (eosinophilic granuloma/Langerhans cell histiocytosis), malignant tumors (Ewing sarcoma and angiosarcoma), inflammatory conditions (eg, apatite- associated destructive arthritis), endocrine disorders (eg, osteolytic hyperparathyroidism), benign non-neoplastic conditions (venous or venolymphatic malformation), and other syndromes that present with osteolysis.1,2 Nevertheless, progressive and unusually substantial bone destruction without evidence of repair is almost pathognomonic for Gorham disease.9
Treatment
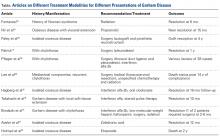
Although no single or combined treatment modality is considered the gold standard (Table),1,2,4,13-23 management of Gorham disease generally centers on radiation therapy for local control of large and painful lesions and on surgical intervention for pathologic progression that would otherwise result in substantial functional limitations.2 Also described for treatment are antiosteoclastic medications (bisphosphonates), which are often used in conjunction with radiation and/or surgical intervention.2,4 The newer literature cites some benefit of using various experimental modalities, including a combination of interferon alfa-2b and low-molecular-weight heparin,13 and even propranolol.14Surgical treatment usually includes lesion resection and subsequent reconstruction using combinations of bone grafts (allogenic) and prostheses. Bone graft alone is quickly resorbed and has not been found to be beneficial.1,2,4,20