The for five common surgical conditions, according to a Jan. 24 report in JAMA Surgery.
“Given current debate on the ACA [Affordable Care Act] and reforms to the Medicaid program, evidence on the effects of these policies is critical ... As policy makers weigh changes to or a potential repeal of the ACA, these findings provide important new data on the early clinical effects of the law’s coverage expansion,” said investigators led by Andrew Loehrer, MD, of the department of surgical oncology at MD Anderson Cancer Center, Houston.
For a baseline, the team used hospital administrative data from the Vizient Clinical Data Base and Resource Manager to assess outcomes for appendicitis, cholecystitis, diverticulitis, peripheral artery disease, and aortic aneurysm in 42 states during 2010-2013, before the ACA took effect in 2014. They then compared outcomes during 2014-2015 in the 27 states that expanded Medicaid programs under the ACA with 15 states that did not. The study included 225,572 hospital admissions in the Medicaid expansion states and 67,957 in the nonexpansion states at more than 200 academic medical centers and affiliated hospitals.
Medicaid expansion in the 27 states was associated with a 7.5-percentage point decreased probability of patients being uninsured (95% confidence interval, –12.2 to –2.9; P = .002) and an 8.6-percentage point increased probability of having Medicaid (95% CI, 6.1-11.1; P less than .001).
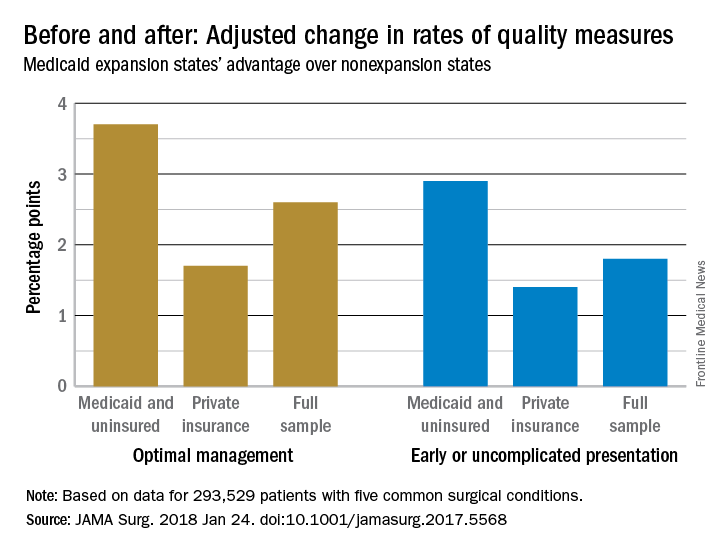
Medicaid expansion was also associated with a 1.8-percentage point increase in the probability of early, uncomplicated presentation (95% CI, 0.7-2.9; P = .001) and a 2.6-percentage point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation (95% CI, 0.8-4.4; P = .006).
“Uncomplicated presentation” meant, for example, diverticulitis without abscess, fistula, or sepsis; unruptured aortic aneurysm; and peripheral artery disease without ulcerations or gangrene. Optimal management included cholecystectomy for acute cholecystitis; laparoscopic approaches for cholecystectomy or appendectomy; and limb salvage for peripheral artery disease.The improvements were concentrated among Medicaid and uninsured patients, who were most likely to benefit from coverage expansion, rather than those with private insurance.
The investigators acknowledged the limitations of their data for tracking changes access and quality of care for surgical patients. “We recognize that the data on improved quality of care are not as clear. Our use of composite outcomes has specific limitations,” they wrote.
“As expected for the conditions studied, our analysis found no significant change in the overall number of individuals treated but rather a change in the timeliness in which individuals received care.” Meanwhile, “our sample revealed an increase in the percentage of surgical patients who were uninsured in nonexpansion states after 2014,” which was associated with “worsening of outcomes ... whereas expansion states had stabilization or improvement,” they said. In Medicaid expansion states, the number of uninsured dropped from 14.% to 6.8%, but in the nonexpansion states, the number of uninsured actually increased slightly from 21.2% to 21.9%.
There was no funding source reported for the study. The authors had no conflicts of interest.
SOURCE: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568