SCOTTSDALE, ARIZ. – A new model for predicting 1-year survival after elective endovascular repair of degenerative thoracic aortic aneurysm suggests that the risks outweigh potential benefits of the procedure in some older patients with multiple comorbidities.
For patients aged 70 years or older who have multiple comorbidities, there is a very high risk of death in the year following thoracic endovascular aortic aneurysm repair (TEVAR), so it may be best to wait until the aneurysm is large enough that the risk from not doing TEVAR outweighs the risk of performing the procedure, according to Dr. Adam W. Beck.
Dr. Beck, of the University of Florida, Gainesville, and his associates analyzed data from a prospective registry of all 526 consecutive TEVARs performed on patients with intact degenerative, asymptomatic thoracic aneurysms at the university between 2000 and 2010. After excluding urgent or emergent cases, the researchers used data from 224 patients who underwent elective TEVAR to identify predictors of death within a year of TEVAR, and compared predictions to survival data from the Social Security Death Index.
Overall, 3% of patients died within 30 days of TEVAR, and 15% died within 1 year – rates that are comparable to those of many studies reported in the medical literature, Dr. Beck said at the annual meeting of the Southern Association for Vascular Surgery.
In a multivariate analysis of factors associated with mortality, being at least 70 years old conferred nearly a sixfold increase in the predicted 1-year risk of death (hazard ratio, 5.8). Patients who had an adjunctive procedure at the time of TEVAR, such as brachiocephalic/visceral stent placement or concomitant visceral debranching procedures, were 4.5 times more likely to die within a year than were patients without an adjunctive procedure.
The predicted risk of death at 1 year was 3 times higher in patients with peripheral vascular occlusive disease and 2.4 times higher in patients with coronary artery disease than in patients without those diseases. All of these associations were statistically significant. The presence of chronic obstructive pulmonary disease showed a nonsignificant trend toward a 1.9-fold higher risk of death at 1 year (P = .06).
Having a diagnosis of hyperlipidemia appeared to be protective, because it was significantly associated with a 60% decrease in the risk of death at 1 year after TEVAR. When the risk prediction model was created, the lack of a history of hyperlipidemia was considered to be a risk factor.
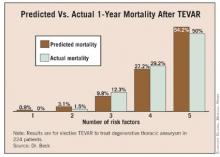
The risk of death at 1 year rose as the number of significant risk factors increased, and predictive risk correlated well with actual mortality data, Dr. Beck said.
In general, aneurysm diameter was larger in patients with more risk factors, and the risk of death at 1 year increased with aneurysm size and number of risk factors, he added.
The risk of rupture, as reported in the previous literature, is approximately 2% for thoracic aortic aneurysms measuring 5.5 cm in diameter, 10% for aneurysms with a diameter of 6.5 cm, 15% for those measuring 7 cm in diameter, and 45% for aneurysms with a diameter of 8 cm.
When the risk of 1-year mortality is plotted against the number of risk factors, it appears that TEVAR should be delayed in patients with three or more risk factors until their aneurysm diameter is greater than the usual 6-cm threshold commonly used to justify the risk of TEVAR, Dr. Beck said.
"This is an important contribution to our literature," said Dr. Hazim J. Safi, a discussant at the meeting. "Most of us implicitly, when we decide how to manage these patients, would categorize the patient by presumed risk," said Dr. Safi, professor and chair of cardiovascular and thoracic surgery at the University of Texas, Houston. "I congratulate the authors for quantifying the relationship between the risk factors and mortality rate."
Usually, surgeons discuss the annual risk of thoracic aneurysm rupture and compare this with the 30-day operative mortality risk when advising patients who are considering TEVAR, Dr. Beck said. To adequately assess the success of aneurysm repair, however, longer survival should be considered, he said.
"It’s important to note that only 21% of deaths within 1 year of repair occurred within 30 days after the procedure, underscoring the importance of looking beyond the first 30 days to determine the benefit of therapy," Dr. Beck said. Even for the groups with multiple risk factors who are at very high risk, the majority of deaths occurred outside the 30-day window.