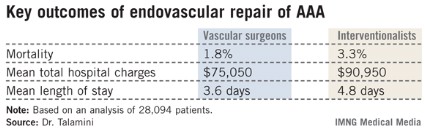
INDIANAPOLIS – Major outcomes in patients undergoing endovascular repair of abdominal aortic aneurysm are superior in terms of mortality, length of stay, and total hospital charges when the procedure is done by vascular surgeons rather than cardiologists or interventional radiologists, according to an analysis of a comprehensive national hospital database.
"Obviously these are striking findings," Dr. Mark A. Talamini noted in presenting the study results at the annual meeting of the American Surgical Association. "We believe that health policy in support of selective referrals for aneurysm repair, or integrating interventionalists and vascular surgeons more effectively, should be considered."
 Courtesy Wikimedia Commons/Milorad Dimic, MD/Creative Commons License
Courtesy Wikimedia Commons/Milorad Dimic, MD/Creative Commons License
Major outcomes in patients undergoing endovascular repair of abdominal aortic aneurysm (above) are superior when the procedure is done by vascular surgeons rather than cardiologists or interventional radiologists, a new analysis shows.
He presented an outcomes analysis involving 28,094 patients who underwent endovascular implantation of a graft for an abdominal aortic aneurysm within the Nationwide Inpatient Sample during 2001-2009. This database, sponsored by the Agency for Healthcare Research and Quality, receives input from a representative cross-section composed of 20% of U.S. hospitals. Dr. Talamini and coworkers were able to reliably determine whether an operator was a vascular surgeon, a cardiologist, or an interventional radiologist. Vascular surgeons performed 78.1% of the cases, while nonsurgeon interventionalists did the rest. Ninety-seven percent of patients presented with a nonruptured aneurysm.
The unadjusted differences in key outcomes between vascular surgeons and interventionalists were striking. Perhaps even more impressive were the differences following adjustment for operator volume, comorbid conditions, aneurysm rupture status, patient demographics and socioeconomic status, and hospital location and teaching status. The interventionalists’ patients had a 39% greater risk of mortality, an average of $20,000 more in total hospital charges, and a 1.4-day longer length of stay, reported Dr. Talamini, a nonvascular surgeon who is professor and chairman of the department of surgery at the University of California, San Diego.
Additional findings of interest were that the patients of high-volume operators (defined as those who performed more than 10 cases per year) had a 31% reduction in mortality risk regardless of operator specialty. In addition, high-volume operators averaged $10,000 per patient less in total hospital charges and shorter hospital length of stay by 1 full day. Undergoing aneurysm repair in a teaching hospital had no impact upon mortality or total charges, but was associated with an average 0.4-day greater length of stay, he continued.
Dr. Talamini offered two potential explanations for the disparate outcomes. One is that perhaps the patient populations of vascular surgeons and interventionalists differ in ways that were not accounted for in the multivariate analysis. The other possibility is that vascular surgeons achieve better outcomes because their training and experience are superior, allowing them to make better judgments about treatment than those of interventionalists.
"Obviously, this is the ‘we’re better than they are’ argument, and I hardly think we can assume that this is the case until we exhaust all other potential explanations. Further work using longitudinal databases with more detail hopefully will allow us to do just that," said Dr. Talamini.
Discussant Dr. K. Craig Kent called the study findings "very provocative."
"The moral of the story is expertise in disease is far more important than expertise in technology," declared Dr. Kent, professor and chairman of the department of surgery at the University of Wisconsin, Madison.
"When I first became a vascular surgeon 25 years ago it was difficult to recruit to the specialty. There were few that wanted to care for a group of patients for whom procedures were long and tedious, reoperations were common, and outcomes weren’t always favorable," Dr. Kent recalled. "Fast forward to 2013, where everybody wants to be a vascular surgeon: cardiologists, interventional radiologists, nephrologists, dermatologists, vascular medicine physicians, and many others. Why the dramatic change? For the nonsurgeons, the reason is the development of minimally invasive technology that has allowed any specialist with catheter-based skills to participate in vascular care. But is it appropriate for nonsurgical specialists to treat vascular patients? The answer from this study is a resounding no."
Dr. Samuel E. Wilson, a vascular surgeon who was Dr. Talamini’s coinvestigator in the study, said he thinks patient selection is the key to understanding the outcome disparities.
"If you think about it, the vascular surgeon in his office has the ability to make an elective decision, carefully considered, and decide whether or not he’s going to actually do the procedure. The hospital-based radiologist may not have that opportunity; he receives a call, a procedure on an inpatient is requested, and he feels obligated to proceed. Another key aspect may be postoperative care. Vascular surgery patients receive their postoperative care under the direction of the surgeon," observed Dr. Wilson of the University of California, Irvine.