DALLAS – Routine screening is warranted for the first-degree relatives of patients who present with thoracic aortic disease before age 60 years in the absence of predisposing conditions such as hypertension, Marfan syndrome, or bicuspid aortic valve, Dr. Elizabeth N. Robertson said at the American Heart Association scientific sessions.
"We’ve shown that screening of first-degree relatives for familial thoracic aortic aneurysm disease is essential, as we detected an average of two additional affected individuals per initial patient," noted Dr. Robertson of Royal Prince Alfred Hospital in Camperdown, Australia.
Thoracic aortic aneurysm and dissection (TAAD) is more common than previously recognized. It accounted for one in seven cases of thoracic aortic disease in a series of 1,276 patients who presented with thoracic aortic disease to the tertiary center during a recent 12-year period.
TAAD is an asymptomatic progressive dilatation of the thoracic aorta characterized by cystic medial necrosis. It has no evident predisposing cause. It can occur sporadically or in a familial form, which has been linked to multiple gene mutations transmitted in autosomal dominant fashion in large family studies. Unlike Marfan syndrome, Ehler-Danlos syndrome, and other genetic causes of thoracic aortic disease, TAAD has no characteristic external physical features. The clinical signs of TAAD are minimal and nonpathognomonic: an aortic flow murmur or a prominent A2 second heart sound.
"The most common first indication of a problem is occurrence of aortic dissection, by which time it’s often too late," she said.
Dr. Robertson and her coinvestigators did a retrospective review of 1,276 patients who presented with thoracic aortic disease at the Royal Prince Alfred Hospital cardiovascular myopathy service during 2000-2012. TAAD was seen in 178. TAAD was defined as aortic dilatation or dissection before age 60 years with no predisposing condition and with confirmation of cystic medial necrosis whenever possible. TAAD was sporadic in 93 patients. The other 85 had familial TAAD based upon their history of having one or more affected family members. Screening was offered to all first-degree relatives of the patients with familial TAAD.
Two-dimensional echocardiographic screening of 383 first-degree family members identified an additional 181 affected individuals, bringing the total study population with familial TAAD to 266. When the screened patients were added to the 93 patients with sporadic TAAD, thoracic aortic aneurysm and dissection became the second most common cause of thoracic aortic dilatation or dissection seen at the hospital during the study period.
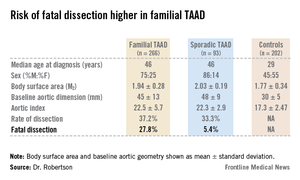
The median age at diagnosis was 46 years both in the sporadic and familial TAAD groups. However, the detection rate was steady from the teen years through old age, underscoring the importance of surveillance of younger at-risk individuals. Most of the at-risk population was male, 73% of the familial and 86% of the sporadic cases. The aortic diameter at diagnosis varied, but it was 50 mm or greater in 25% of the subjects in the familial and sporadic groups. Under current guidelines, this measure warrants semi-urgent surgical intervention.
Of the first-degree relatives identified through screening, 26% experienced aortic dissection, as did more than 60% of the initial 85 probands with familial TAAD. The familial phenotype appears to be more aggressive: 40% of patients with familial TAAD who had an aortic dissection died as a result, compared with less than 15% of patients with sporadic TAAD who had aortic dissection.
Dissection in patients with familial TAAD frequently occurred at smaller aortic diameters, including less than 40 mm. Dr. Robertson noted this width would not typically be flagged as a problematic in routine screening.
The rate of progression of dilatation in patients with familial TAAD was 0.5 mm per year, which is roughly half the rate typically seen in patients with Marfan syndrome, according to Dr. Robertson.
Session cochair Dr. Brendan M. Everett, director of the general cardiology inpatient service at Brigham and Women’s Hospital, Boston, called Dr. Robertson’s study "fascinating" and thanked her for bringing to his attention a serious and relatively common condition he was hitherto unaware of. Given that aortic size is age-, gender-, and body surface area–dependent, what’s the best threshold aortic diameter in defining a positive screening test in first-degree relatives?, he asked.
Because of those associations, Dr. Robertson replied, the best definition of a positive screening test is a Z score greater than 2, rather than simply relying upon a given aortic diameter measurement.
Dr. Robertson’s study was conducted free of commercial support. She reported having no financial conflicts of interest.