Glomus tumors are neoplasms that originate from normal glomus bodies in the skin and are most commonly found in the subungual areas of the digits.1 Glomus bodies are neuromyoarterial structures in the reticular dermis that serve as specialized arteriovenous anastomoses. These bodies contain afferent arterioles and efferent veins with multiple connections, and glomus cells have contractile properties because of their similarity to smooth muscle cells.1,2 Glomus bodies help regulate blood flow and temperature of the skin and are found in their largest concentration in the fingertips, palms of the hands, and soles of the feet.3,4
Glomus tumors represent hyperplastic glomus bodies and make up 1% to 4.5% of upper extremity neoplasms, with approximately 75% in the hand and 50% in the subungual area.1,5,6 These tumors can also present in multiple locations at once and can occur in atypical and ectopic locations.3 Although generally benign, glomus tumors can also exhibit malignant and metastatic potential in rare cases.7,8 They can also be locally aggressive with bony destruction of the distal phalynx.2,9,10 Tumors typically present as painful solitary soft-tissue lesions that are exquisitely tender to palpation, dark red-purple or bluish, and hypersensitive to cold.5,10 Van Geertruyden and colleagues10 reported that the diagnosis of glomus tumor can be made clinically in 90% of cases. However, glomus tumors can easily be mistaken for other lesions, such as hemangiomas, angiomas, neuromas, neurofibromas, lipomas, and ganglion cysts. An inaccurate or incomplete workup can result in persistent pain and symptoms along with intraoperative complications.3 Magnetic resonance imaging (MRI), the most sensitive imaging modality for detecting glomus tumors of the hand, can assist in the workup.3,11,12
Extradigital glomus tumors are difficult to diagnose because of their rarity and unspecific symptoms and presentation.13 Misdiagnosis and delayed diagnosis can result in significant chronic pain, disuse syndromes, and disability.1,10 Correct diagnosis and surgical resection are generally curative with complete resolution of symptoms.
In this article, we report a case of a large atypical glomus tumor that occurred on the wrist and involved the radial artery. This tumor was successfully treated with surgical excision. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 63-year-old man presented to clinic with an extremely tender soft-tissue mass on his nondominant, left wrist. The mass had been increasing in size for a year. It was painless at rest but very painful to light palpation, with referred pain proximally up to the shoulder.
The patient did not recall any traumatic or inciting event, had not undergone any prior workup or treatment for symptoms, and had no history of masses elsewhere on the body. Past medical history was significant for type 2 diabetes and colon and prostate cancer, which had been treated with chemotherapy and was now in remission.
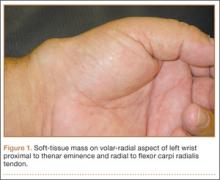
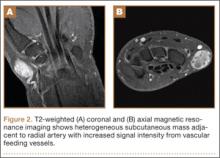
Physical examination revealed a 2×2.5-cm well-circumscribed soft-tissue mass on the volar-radial aspect of the left wrist proximal to the thenar eminence and radial to the flexor carpi radialis tendon (Figure 1). The mass was soft, mobile, and nonfluctuant and did not transilluminate. The overlying skin was normal in color and appearance—no discoloration, erythema, wounds, or drainage. The radial artery was palpable, and the mass did not pulsate or have a bruit. The patient had normal wrist range of motion limited by pain on compression of the mass with motor and sensation intact throughout the hand. Plain radiographs of the wrist showed no bony pathology or involvement from the mass. A soft-tissue shadow was visible around the wrist without calcifications. A wrist MRI was performed to better evaluate the mass, and the T2-weighted images showed a heterogeneous subcutaneous mass adjacent to the radial artery with increased signal intensity from surrounding feeding vessels (Figure 2).
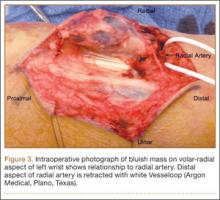
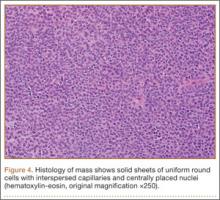
Given the clinical and imaging findings, there was concern for a possible vascular tumor. Therefore, excisional biopsy was recommended over needle biopsy because of the bleeding risk. With the patient under general anesthesia, and a tourniquet used without exsanguination, a Brunner-type zigzag incision was made centered over the mass with elevated skin flaps. The 2.7×2.6×1.1-cm mass was superficial and involved the radial artery (Figure 3). After the radial artery was dissected proximally and distally, 2 perforating vessels were found entering the mass. These vessels were ligated, which allowed the mass to be peeled completely off the artery. Histology with hematoxylin-eosin staining showed solid sheets of uniform round cells with interspersed capillaries and centrally placed nuclei without evidence of malignancy (Figure 4).
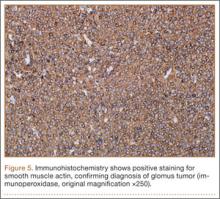
The tourniquet was released before skin closure, and adequate hemostasis was obtained. The wound was closed, and the patient was placed in a volar wrist splint for immobilization. Pain relief after excision of the mass was immediate, and the postoperative course uneventful. After surgery, immunohistochemistry of the mass showed minimal mitotic activity, with a positive immunoperoxidase stain for smooth muscle actin confirming a diagnosis of glomus tumor (Figure 5). At 3-year follow-up, the patient had no pain, symptoms, or tumor recurrence.