Gross Analysis
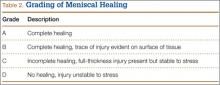
Immediately after specimen removal, all medial menisci were evaluated for gross morphology. A grading system was used for organization and classification of data (Table 2). Three blinded orthopedic surgeon-observers performed all grading. Grade A was considered complete healing of the meniscus. Grade B involved complete healing with a trace of injury remaining on the surface of the meniscus. Grade C represented incomplete healing with a full-thickness injury that was stable to stress of the repair site with an arthroscopic probe. Grade D had no healing with the injured region unstable to stress of the repair site with an arthroscopic probe.
Histologic Analysis and Microscopic Grading of Meniscal Healing
After gross evaluation by the 3 blinded observers, each meniscus was fixed for 24 hours in 10% buffered formalin. Each specimen was then embedded in paraffin and cut into 6-µm slices along the radial plane. The tissue samples were stained with hematoxylin-eosin, and microscopic grading was assigned. The grading system was the same as that used for gross morphologic analysis.
Biochemical Analysis
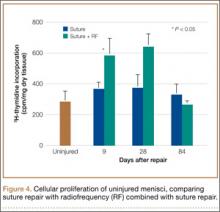
To determine whether RF treatment stimulated a healing response in the avascular zone of the meniscus, measurements of specific biochemical markers were analyzed at 9, 28, and 84 days after treatment. As a control, unrepaired meniscal tissue from the contralateral knee was also analyzed. 3H-thymidine incorporation into the meniscus was measured to assess cell proliferation.23 At sacrifice, control and treated menisci were dissected and immediately placed into sterile culture media (Dulbecco’s modified Eagle’s medium containing 10% fetal bovine serum, antibiotic, and fungicide). 3H-thymidine was added at a concentration of 5µCi/mL of media to each tube. After incubation for 48 hours at 37°C under 5% CO2, the menisci were removed and dialyzed against water for 24 hours to remove unincorporated thymidine. After washing, the menisci were lyophilized, aliquots weighed, and radioactivity determined by liquid scintillation spectrometry. Results are expressed as counts per minute per mg dry tissue weight.
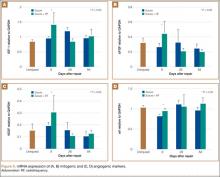
Semiquantitative reverse transcription polymerase chain reaction (RT-PCR) was used to determine mRNA expression of mitogenic growth factors, IGF-1 and bFGF, and angiogenic markers, αV and VEFG.24 National Institutes of Health (NIH) image-analysis software (version 1.61; NIH, Bethesda, Maryland) was used to quantitatively scan RT-PCR profiles after agarose gel electrophoresis and ethidium bromide visualization. Values were normalized to the housekeeping gene, GAPDH.
Statistical Analysis
Data are expressed as mean (SD) and evaluated using an unpaired Student t test between groups. Statistical significance was established at P < .05.
Results
Gross Morphology
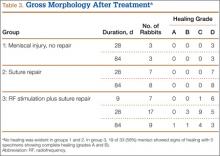
Analysis of gross morphology showed signs of healing only in the group treated with suture repair combined with RF treatment (Table 3). In group 1 (meniscal injury only) and group 2 (suture repair only), no healing occurred at 28 and 84 days (Figure 3A). A meniscal grading system was developed to better describe the varying levels of healing shown in the suture-plus-RF-treatment group (Table 2). Of the specimens that showed healing in group 3, 1 had complete healing (grade A) within the avascular zone of the meniscus at 84 days (Figure 3B). In addition, 4 specimens subjected to suture repair and RF treatment had complete healing with only a trace of injured tissue remaining (grade B). Fourteen specimens in group 3 had incomplete healing with lesions stable to stress suggesting early signs of healing (grade C). In total, 58% of menisci treated with RF showed signs of healing while the remaining 14 specimens in group 3 showed none (grade D).
Histologic Examination
The histology correlated well with gross analysis. No microscopic evidence of healing was seen in groups 1 and 2 (Figure 3C). Of the specimens treated with suture repair combined with RF, 19 (58%) showed varying degrees of histologic healing. While gross morphologic examination showed that only 1 specimen had complete healing, microscopic analysis showed that 1 specimen from group 3 had grade B healing on gross analysis but grade A healing on histologic analysis. Thus, upon histologic examination, 2 specimens showed complete healing of injuries in the avascular zone of the meniscus when treated with suture repair combined with RF treatment rather than the 1 specimen seen on gross morphology (Figure 3D).
Biochemical Analysis
Biochemical assessments were performed at 9, 28, and 84 days after surgery. 3H-thymidine incorporation was studied as a marker for cellular proliferation, and its levels were significantly higher in meniscus explants treated with RF (Figure 4). The mean (SD) rate of incorporation for meniscal tears treated with suture repair plus RF was 590 (80) cpm/mg dry tissue at 9 days. This value was approximately 40% greater than the menisci treated with suture repair only, which had a mean (SD) value of 380 (30) cpm/mg (P < .05). Normal, unrepaired meniscal tissue had a mean (SD) 3H-thymidine incorporation rate of 250 (35) cpm/mg. By 84 days, thymidine levels returned to uninjured levels in both suture-only and RF-treated menisci. Semiquantitative RT-PCR analysis showed that, 9 days after repair, the RF-treated menisci had increased mRNA expression of IGF-1, bFGF, VEGF, and αV relative to untreated repairs (Figure 5). There was a statistically significant acute phase response in IGF-1, bFGF, VEGF and αV in groups treated with RF at 9 days (P > .05).