Discussion
This retrospective analysis explored how day of the week of primary THA affected LHS. Various confounders, such as surgery and patient factors, were also examined so that the multivariate analysis would be able to isolate the effects of surgical day of the week on LHS.
Effect of day of the week of primary THA on LHS was not investigated in the United States before. In Denmark, in a study similar to ours, Husted and colleagues4 found a 400% increase in the probability of LHS of more than 3 days when patients operated on a Thursday were compared with patients operated on a Friday. The authors reasoned that the Thursday patients most likely had a compromised physical therapy protocol owing to the inclusion of weekend days in the crucial postoperative period. LHS was consequently increased so that these patients would achieve their therapy goals before being discharged. Our investigation showed that LHS did not differ significantly by surgical day of the week. Although patients who had THA on a Thursday had 15% longer LHS than patients who had THA on a Monday, this difference was not statistically significant (P = .496), even though the study was adequately powered to detect a change in LHS of a whole day.
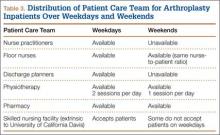
Table 3 summarizes the difference in quantum of workforce on weekdays and weekends at our center. The physiotherapy sessions were reduced to 1 per day. Nurse practitioners and discharge planners were not available on weekends, and some skilled nursing facilities and rehabilitation centers refused to accept patients on weekends. At our center, a teaching institute, the clinical duties of discharge planners and nurse practitioners were assumed by licensed physicians (orthopedic residents covering the arthroplasty team on weekends). This could be one of several possible reasons our study failed to detect statistically significant difference between the 2 groups. This kind of alternative arrangement may not be possible at many other centers. However, our study results provide a reasonably accurate logistical aim with regard to workforce availability on weekends to keep LHS in check.
The importance of giving patients an inpatient physical therapy regimen in timely fashion has been demonstrated in other studies. Munin and colleagues,9 in a randomized controlled trial, evaluated 71 patients who underwent elective hip and knee arthroplasty and received 2 different physical therapy regimens. Patients started their in-treatment physical therapy on postoperative day 3 or 7. Mean total LHS was shorter in the 3-day group (11.7 days) than in the 7-day group (14.5 days) (P < .001). Brusco and colleagues10 also showed that introducing weekend physical therapy services significantly reduced LHS in patients who underwent THA (10.6 vs 12.5 days; P < .05). Rapoport and Judd-Van Eerd11 retrospectively analyzed orthopedic surgery LHS, comparing patients treated in a community hospital during a period of 5-days-a-week physical therapy coverage and patients treated during a period of 7-days-a-week physical therapy coverage. The 7-days-a-week group had significantly statistically shorter mean LHS.
Another rationale for analyzing the impact of surgical day of the week stems from the expectation that patients who undergo THA on Wednesday or Thursday and are scheduled to have physical therapy or be discharged on the weekend may be affected not only by reduced inpatient weekend physical therapy coverage but also by difficulties in being transferred to a skilled nursing facility or rehabilitation center if not discharged home. In our study, the patients who were to be discharged to a rehabilitation center were delayed by 12.5%, and this statistic trended toward significance (P = .061). Our literature search did not turn up any studies, US or European, specifically linking LHS to discharge disposition (whether patient is discharged home or to a skilled nursing facility or rehabilitation center).
Reduced medical staffing on weekends may not only affect the quality of in-hospital patient care but may also result in unnecessary delays in discharge. Chow and Szeto12 retrospectively analyzed the medical records of all acute medical wards in a university hospital and compared weekend discharge rates before and after implementation of a work ordinance, which decreased the physician workforce by half on Saturday and Sunday. Results showed a 2.7% decrease in the weekend discharge rate after the work ordinance was established. The number of weekday discharges between the 2 time periods did not differ. Increasing the workforce availability presents a challenge in academic medical centers where graduate medical education enforces a strict cap on resident duty hours. Under these circumstances, a more feasible approach to decreasing LHS for THA patients is for surgical planning committees to provide the joint replacement services with operative block times early in the workweek.