Results
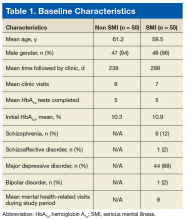
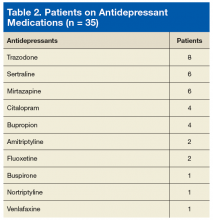
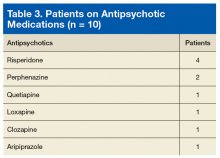
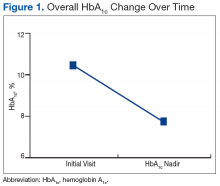
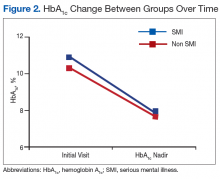
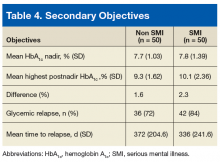
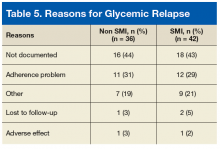
A total of 134 veterans who were referred to the RN CDE/PharmD clinic were reviewed from January 1, 2011 to December 31, 2014 with 50 veterans in the SMI group and 50 veterans in the non-SMI group. The mean age, gender, number of clinic visits, number of HbA1c tests, and mean initial HbA1c were similar between groups (Table 1). Veterans in the SMI group were followed by the clinic longer than veterans without SMI (298 d vs 239 d, respectively) and had a slightly higher baseline HbA1c (10.9% vs 10.3%). The majority of veterans in the SMI group had MDD (88%), and the mean number of mental health-related visits was 8 visits per veteran. Most veterans were prescribed antidepressants during the study period (70%), with fewer veterans prescribed antipsychotics (20%). Concurrent antidepressant and antipsychotic medications used during the study period are detailed in Tables 2 and 3. Overall, there was a significant decrease in mean HbA1c of 2.8% (10.6% to 7.8%; P < .001) for the entire study population (Figure 1). Veterans with SMI had a greater reduction in HbA1c (SMI 3.0% vs non-SMI 2.6%, P = .271) (Figure 2). Secondary objectives are listed in Table 4. The mean HbA1c nadir was similar between groups (SMI 7.8% +/- 1.39% vs non-SMI 7.7 +/- 1.03%); however, the mean highest postnadir HbA1c was higher in the SMI group compared with that of non-SMI (9.3% +/- 1.62% vs 10.1% +/- 2.36%), with a difference of 1.6% vs 2.3% (P < .005). Eighty-four percent of veterans in the SMI group relapsed compared with 72% of veterans without SMI, which was not a significant difference. Of the veterans who relapsed, the mean time to relapse was longer in the veterans without SMI compared with that of veterans with SMI, but the difference was not significant (372 +/- 204.6 d vs 336 +/- 241.6 d, P = .772). The most common documented reason for glycemic relapse was nonadherence to medications or diet (Table 5).Discussion
Collaborative interventions have improved glycemic control in patients with concurrent SMI and DM. Although there was not a significant difference in mean HbA1c from the initial HbA1c to the nadir HbA1c between study groups, this study provided valuable insight for the RN CDE/PharmD clinic. The mean HbA1c decreased over time in both study groups, demonstrating that the collaborative intervention was effective in improving glycemic control in veterans with SMI and veterans without SMI. The mean HbA1c decrease in the SMI group was slightly higher compared with that of the non-SMI group, but the difference was not significant. The decrease in mean HbA1c also demonstrated that the RN CDE/PharmD interventions were effective in each group. Contrary to this study’s hypothesis that veterans with SMI would have worse glycemic control compared with that of veterans without SMI, this study demonstrated that there was no difference in glycemic control between groups.
Veterans in the SMI group had a significantly greater percentage increase in mean HbA1c postnadir, indicating that their glycemic control worsened postnadir compared with that of the non-SMI group. If veterans with SMI relapsed, they tended to relapse to a greater extent compared with veterans without SMI, as indicated by a larger percentage increase in mean HbA1c. Time to relapse was shorter in veterans with SMI compared with that of veterans without SMI, but the difference was not significant. Using the information gathered, if veterans with SMI relapsed, they tended to relapse sooner and with a greater percentage increase in HbA1c compared with that of veterans without SMI.
Limitations
As a retrospective study, data collection was limited to the information found in the veteran’s EMR: Data collected were dependent on accurate and comprehensive documentation in the veteran’s problem list and progress notes. Additionally, the time between HbA1c tests was not analyzed when determining the differences in mean HbA1c. These data may be helpful in identifying reasons for glycemic relapse. Glycemic relapse depended on the number of HbA1c tests that the veteran completed. Time to glycemic relapse may occur sooner in veterans who completed more frequent HbA1c testing.
Conclusion
There was a significant decrease in mean HbA1c for the entire group over time. In comparing the percentage change in mean HbA1c between groups, there was not a significant difference in the decrease in mean HbA1c from initial to nadir HbA1c in veterans with SMI compared with that of veterans without SMI. However, veterans with SMI had a significantly larger increase in HbA1c postnadir compared with that of veterans without SMI, indicating that support would likely be needed after the veteran achieves his or her HbA1c target. Strategies such as extending the follow-up time in the RN CDE/PharmD clinic, expanding collaborative services with behavioral medicine and psychiatry, additional shared medical appointments or support groups for veterans with DM and SMI, and health literacy assessments may need to be adapted to assist in maintaining glycemic control in veterans with concurrent SMI and DM.