• Is the patient actually bolusing for meals? Does the patient check blood glucose postprandially and bolus when the reading is high?
PATIENT TRAINING BEFORE PUMP INITIATION
Insurance coverage is generally favorable for pumps and associated supplies, since their cost benefit (ie, decreases in use of antidiabetic drugs and of health care resources6) is well proven for patients with type 1 diabetes. For those with type 2 diabetes, obtaining coverage is more challenging5 but can be supported if the patient has a history of severe hypoglycemia, insulin resistance, or uncontrolled blood sugar levels.6,7
Pump manufacturers employ insurance specialists to work with patients and providers in order to facilitate the insurance reimbursement process. Payment plans are available for what insurance does not cover, and pump warranties last for several years. Many insurance plans do not cover an automatic upgrade to a newer pump when the warranty expires, but the patient may be eligible for a discount on a newer pump.
Before initiating pump use, patients receive instruction from certified pump trainers—generally health professionals, such as nurses and registered dietitians, who may be employees of the endocrine practice or of the pump manufacturing company, or independent contractors; many are certified diabetes educators (CDEs). Training may be conducted in the patient’s home or in the medical office. Typically, patients are given some sort of DVD or CD-ROM and workbook to complete before pump training takes place.
Pump trainers make sure patients understand the basics of carbohydrate-counting, sick day management, and treatment of hypoglycemia and hyperglycemia. Training may comprise two sessions, one during which the patient can wear the pump with a saline administration and practice with it for a few days before starting on insulin at the second session. Training should be individualized to allow for different speeds and styles of learning.
Careful patient selection is the key to successful pump use. Optimally, patients should be motivated to improve their blood glucose control, compliant with their current regimen, and proficient in their diabetes self-management skills, including carbohydrate-counting, troubleshooting, and making adjustments for day-to-day variability in their circumstances.8
Pump trainers can make suggestions to the patient’s diabetologist regarding basal rates, correction factors, and insulin-to-carbohydrate ratios, but a health care provider’s order is necessary to initiate use of a pump.
RESOURCES FOR PATIENTS
Referral to a CDE and/or an endocrinology specialist may be helpful for any patient who was started on a pump in the past but is now struggling with management or would like to fine-tune his or her control. Patients who are unable to reduce an A1C of 8% may also benefit from referral. Not all of these practitioners operate at an expert level in pump therapy, however.
Given the shortage of endocrinologists and CDEs, especially in rural areas, finding a qualified practitioner is sometimes challenging. The American Association of Diabetes Educators maintains a referral service at www.diabeteseduca tor.org/find or (800) TeamUp4.
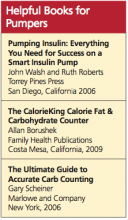
Patients can also contact the pump manufacturer to ask about local resources. Classes in advanced pumping skills and local pump support groups are often sponsored by pump manufacturers. Additionally, excellent books have been published on pump therapy and carbohydrate-counting, including those listed below.
RISKS AND BENEFITS OF INSULIN PUMP THERAPY
Risks of insulin pump therapy include DKA, infusion-site problems, and infection leading to abscess.27,33,34
In the absence of insulin, patients with type 1 diabetes produce ketones; because a pump uses only rapid- or short-acting insulin, a failure to deliver that insulin can lead to acute insulin deficiency, resulting in DKA. All pumps are equipped with pressure-sensitive alarms that will alert the user to a blockage that may result in failure to deliver insulin. Pump users who receive low doses of insulin (the absence of which may not cause sufficient pressure to trigger the alarm) or who experience pump blockages that cause only partial delivery may experience alarm failure. It is crucial for patients to monitor their blood sugar frequently; those who are unwilling to do so are not good candidates for insulin pump therapy.8
Infusion-site problems can include skin reactions to tape or infections resulting from inadequate cleansing or from failure to cleanse the site and change the infusion set, as recommended by the manufacturer, every two to three days. Pump trainers or the pump manufacturer’s customer service team can offer solutions to infusion-site skin care problems. Scrupulous handwashing, timely site changes, and cleansing of the skin are essential to preventing site problems.
Benefits of insulin pump therapy include the opportunity to individualize therapy for specific medical needs and lifestyle differences. Basal profiles can be individually adjusted for metabolic concerns, such as the dawn phenomenon or temporary illness—as well as day-to-day changes, such as increased physical activity. Bolus calculators allow for more accurate matching of the insulin-to-carbohydrate ratio and the amount of correction insulin necessary before meals.