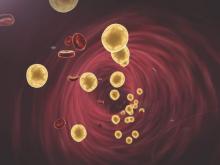
Adding ezetimibe to atorvastatin boosted the regression of coronary plaque in patients with elevated cholesterol who had just undergone percutaneous coronary intervention (PCI) for acute coronary syndromes or stable angina, according to a report published July 27 in the Journal of the American College of Cardiology.
Compared with atorvastatin monotherapy, the dual-agent lipid-lowering strategy also improved vascular remodeling in the targeted artery segments to a much greater degree in the prospective, multicenter trial known as PRECISE-IVUS (Plaque Regression With Cholesterol Absorption Inhibitor or Synthesis Inhibitor Evaluated by Intravascular Ultrasound).
“Our positive results from the PRECISE-IVUS trial could lead to an early reevaluation of the new [American College of Cardiology/ American Heart Association] lipid management guidelines that endorses statins as the only recommended drugs for treating cholesterol-related CV risk,” wrote Kenichi Tsujita, M.D., Ph.D., of Kumamoto University in Japan, and his associates.
The study findings also confirm that adding ezetimibe can be beneficial for patients who are unable to tolerate high-dose statins, as well as for those who don’t achieve adequate cholesterol control despite maximal statin therapy.
The investigators compared atorvastatin monotherapy against atorvastatin plus ezetimibe in 246 adults who underwent PCI under intravascular ultrasound guidance at 17 cardiovascular centers. The participants had LDL-cholesterol levels of more than 100 mg/dl and were randomly assigned to receive either atorvastatin plus ezetimibe (122 patients) or atorvastatin alone (124 patients) for 9-12 months, at which time they underwent repeat intravascular ultrasound imaging.
The primary end point – the absolute decrease in percent atheroma volume of the selected coronary segment – was superior with dual therapy (1.4% vs. 0.3%), and a significantly greater percentage of patients in the dual-therapy group showed coronary plaque regression (78% vs. 58%).
These between-group differences were most pronounced in the subset of patients with acute coronary syndromes, Dr. Tsujita and his associates wrote (J. Am. Coll. Cardiol. 2015; 66: 495-507 [doi:10.1016/j.jacc.2015.05.065]).
But despite the beneficial effect of combination therapy on coronary plaque, the frequencies of adverse cardiovascular events and the rates of target-vessel revascularization were similar between the two study groups.
The study was supported in part by the Japanese Ministry of Education, Science, and Culture. Dr. Tsujita reported having no relevant financial disclosures; his associates reported ties to Bayer, Boehringer Ingelheim, Daiichi-Sankyo, MSD, Pfizer, Takeda, Novartis, AstraZeneca, Astellas, Bristol-Myers Squibb, Chugai, Dainippon Sumitomo Pharma, Kowa, Ostuka, Sanofi, and Shionogi.