Over the past 3 decades surgery for aortic root replacement has seen a dramatic decline in rates of death and complications, but there have been few studies comparing which technique would be best for specific patients, and those that have been done have been limited by selection bias or small patient numbers.
But a team of investigators from Weill Cornell Medical College in New York have analyzed results of three different aortic root replacement (ARR) procedures over a 17-year period and found that the rates of death during surgery and complications were less than 1% regardless of the technique. They published their results in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1120-9).
“In the current era, aortic root replacement can be performed with very low perioperative risk in high-volume aortic centers,” said Dr. Mario Gaudino and coauthors. “The type of operation performed does not affect early or late survival.”
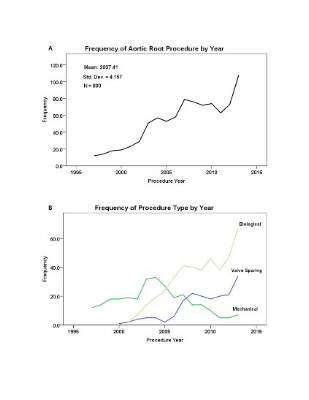
They compared results of three different approaches to ARR performed in 890 consecutive patients in their institution from May 1997 to January 2014: mechanical composite valved graft (mCVG) in 289 patients; biologic composite valved graft (bCVG) in 421; and valve-sparing reconstruction (VSR) in 180. Then the researchers applied propensity matching to neutralize the differences in the baseline characteristics between the different procedures.
The overall rate of death from the operation was 0.2%, but the two patients who died did so in the first 5 years of the study. There were no deaths in the VSR group, and the incidence of complications after surgery was less than 0.5%. Three-year survival was 94.8% and 5-year survival was 89.4%, and reintervention rates at 5 years were 0% for the mCVG group, 2.4% for the bCVG group, and 7.3% for those who had VSR. “Although mCVG remains the gold standard for durability, bCVG and VSR are excellent options for those who either cannot take or wish to avoid long-term anticoagulation,” Dr. Gaudino and colleagues said.
At the time of surgery, 332 patients (37.3%) had at least one associated cardiac procedure, led by arch replacement (149 patients) and coronary artery bypass (81 patients). Eighty-four patients (9.4%) had two or more associated procedures. The bCVG and mCVG groups had the highest rates of associated cardiac procedures.
Before propensity matching, bCVG patients were older and had more comorbidities and worse functional class, while the mCVG group had higher rates of redo procedures and urgent or emergent operations. Connective tissue disorders were most common in the VSR group.
The results paralleled data from the Society of Thoracic Surgery’s Adult Cardiac Surgery Database, Dr. Gaudino and colleagues said, including a fivefold increase in the number of root replacements performed annually during the study period and a shift away from the traditional mCVG operation to widespread adoption of the bCVG and VSR procedures in the later years of the study.
“Surgeons with extensive experience in aortic surgery can tailor their choice of ARR to the procedure that best suits the individual patient based on their baseline characteristics,” Dr. Gaudino and coauthors said.
Dr. Gaudino and his coauthors had no disclosures.