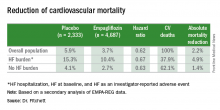
The dramatic reduction in cardiovascular death and heart failure hospitalization seen during treatment with empagliflozin (Jardiance) in the EMPA-REG OUTCOME (Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients) trial, for example, has prompted some cardiologists in the year since the first EMPA-REG report to become active prescribers of the drug to their patients who have type 2 diabetes and cardiovascular disease. The same evidence has driven other cardiologists who may not feel fully comfortable prescribing an antidiabetic drug on their own to enter into active partnerships with endocrinologists to work as a team to put diabetes patients with cardiovascular disease on empagliflozin.
“I hear from more cardiologists who are prescribing empagliflozin, but there still is considerable resistance for prescribing it for several reasons; the primary reason is that they don’t want to be involved in managing diabetes,” David Fitchett, MD, said during an interview at the annual congress of the European Society of Cardiology (ESC). That’s understandable because “most cardiologists do not want to serve as the primary care physician for patients with diabetes, but the least cardiologists can do is prescribe [diabetes] agents with benefits” documented for cardiovascular-disease endpoints, specifically the sodium-glucose cotransporter (SGLT)-2 inhibitor empagliflozin and the glucagon-like peptide (GLP)-1 analogue liraglutide (Victoza), which showed significant benefit for reducing the rate of cardiovascular death, nonfatal MI, or nonfatal stroke in the LEADER (Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results) trial (N Engl J Med. 2016;375:311-22). (Reduction in adverse cardiovascular disease outcomes were also shown in patients with type 2 diabetes as a result of treatment with semaglutide, another GLP-1 analogue not yet approved for U.S. marketing).Endocrinologists generally agree that the recent positive cardiovascular results from large antidiabetic drug trials are repositioning these drugs in the antihyperglycemic algorithm. They see this new glycemic activism by some cardiologists as encouraging but also potentially problematic if physicians not experienced in glycemic control start unilaterally tinkering with a patient’s antidiabetic regimen.In Dr. Fitchett’s practice, “if a patient with type 2 diabetes has an endocrinologist, then I will send a letter to that physician saying I think the patient should be on one of these drugs,” empagliflozin or liraglutide, he said. “If the patient is being treated by a primary care physician, then I will prescribe empagliflozin myself because most primary care physicians are not willing to prescribe it. I think more and more cardiologists are doing this. The great thing about empagliflozin and liraglutide is that they do not cause hypoglycemia and the adverse effect profiles are relatively good. As long as drug cost is not an issue, then as cardiologists we need to adjust glycemia control with cardiovascular benefit as we did years ago with statin treatment,” explained Dr. Fitchett, a cardiologist at St. Michael’s Hospital in Toronto and a senior collaborator and coauthor on the EMPA-REG study.
When results from the 4S [Scandinavian Simvastatin Survival Study] came out in 1994, proving that long-term statin treatment was both safe and increased survival in patients with coronary heart disease, “cardiologists took over lipid management from endocrinologists,” he recalled. “We now have a safe and simple treatment for glucose lowering that also cuts cardiovascular disease events, so cardiologists have to also be involved, at least to some extent. Their degree of involvement depends on their practice and who provides a patient’s primary diabetes care,” he said.
Cardiologists vary on empagliflozin
Other cardiologists are mixed in their take on personally prescribing antidiabetic drugs to high-risk patients with type 2 diabetes. Greg C. Fonarow, MD, has also aggressively taken to empagliflozin over the past year, especially for his patients with heart failure or at high risk for developing heart failure. The EMPA-REG results showed that empagliflozin’s potent impact on reducing cardiovascular death in patients linked closely with a reduction in heart failure hospitalizations. In his recent experience, endocrinologists as well as other physicians who care for patients with type 2 diabetes “are often reluctant to make any changes [in a patient’s hypoglycemic regimen], and in general they have not gravitated toward the treatments that have been shown to improve cardiovascular outcomes and instead focus solely on a patient’s hemoglobin A1c,” Dr. Fonarow said in an interview at the recent annual meeting of the Heart Failure Society of America.