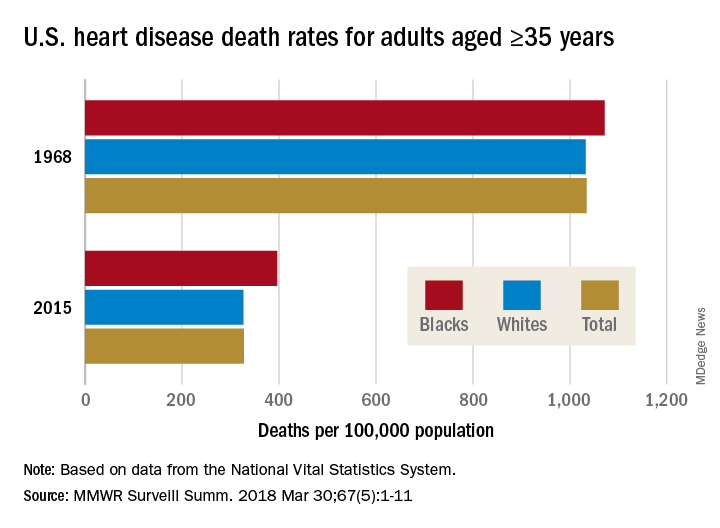
The overall death rate from heart disease is down 68% since 1968 in the United States, but the disparity between blacks and whites has increased over that time, according to the Centers for Disease Control and Prevention.
Overall, heart disease mortality for adults aged 35 years and older went from 1,035 per 100,000 population in 1968 to 327 per 100,000 in 2015, a drop of 68%. For whites, the story was very similar: The death rate dropped from 1,032 to 326, or 68%. For blacks, who had a higher death rate to begin with, at 1,072 per 100,000, the drop was 63% to 396 per 100,000, Miriam Van Dyke, MPH, of Emory University, Atlanta, and her associates reported in MMWR Surveillance Summaries.
Data from the National Vital Statistics System show that “heart disease death rates among blacks and whites decreased at comparable rates during the early portion of the study (1968 until the late 1970s) but then diverged from the late 1970s until the mid-2000s,” when decreases slowed among blacks but not whites, they said. The disparity reached its peak in 2005, reflecting “a larger rate decrease among blacks than whites” since then.Disparities can be seen at the state level as well. For blacks aged 35 years and older, heart disease death rates ranged from 200 per 100,000 in Oregon to 516 per 100,000 in Arkansas in 2015. For whites in that age group, the death rate was lowest in the District of Columbia (198 per 100,000) and highest in Oklahoma (446 per 100,000), Ms. Van Dyke and her associates wrote.
To help them pinpoint differences by race within geographic areas, the investigators calculated ratios of black to white heart disease death rates. In 1968, the state with the highest ratio, or the largest excess of black mortality, was Rhode Island at 1.38, and the state with the lowest ratio, meaning the largest excess of white mortality, was Minnesota at 0.64. There were 27 states that year with a ratio over 1.0, 12 states with a ratio below 1.0, 1 state with a ratio of 1.0 (Wisconsin), and 11 states that did not have a black population large enough to make a reliable estimate, they said.
In 2015, the jurisdiction with the largest excess of black mortality was D.C., with a ratio of 2.42; the state with the lowest ratio was Rhode Island, at 0.69. That year, there were 34 states with a ratio over 1.0, 6 states with a ratio below 1.0, and 11 states – the same 11 as in 1968 – with black populations too small to reliably estimate death rates, the investigators noted.
“The elimination of racial disparities in heart disease death rates, along with continued decreases in heart disease death rates for all persons in the United States, is important for the overall state of health. The trends in black-white disparities in heart disease death rates … highlight the importance of continued surveillance of these trends at the national and state level,” the investigators wrote.
SOURCE: Van Dyke M et al. MMWR Surveill Summ. 2018 Mar 30;67(5):1-11.