CHICAGO – Recent cuts in the door-to-balloon time for treating patients hospitalized with an acute myocardial infarction came with the cost of increased "false alarm" activations of the hospital’s emergency coronary-catheterization laboratory team.
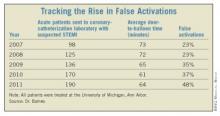
At the University of Michigan, the rate of coronary-catheterization lab activations that proved unnecessary because patients did not have ST-elevation myocardial infarctions (STEMI) jumped from 23% of all activations in 2007 to 48% in 2011, Dr. Geoffrey D. Barnes and his associates reported in a poster at the annual meeting of the American College of Cardiology.
This spike in false-alarm activations coincided with a reduction in the average time to route patients with suspected STEMI from their entry to the hospital’s emergency department to the catheterization lab to start their percutaneous intervention (the "door-to-balloon" time) from 73 minutes in 2007 to 64 minutes in 2011. The concurrence of these two trends was more than coincidence, Dr. Barnes said.
"In 2006, the American Heart Association launched its door-to-balloon initiative [Circulation 2006;113:2152-63], so we looked, starting in 2007," to see how efforts to cut door-to-balloon time affected false activations. "In 2007, our door-to-balloon time was in the 70s [minutes] and we cut the time by an average of about 10 minutes per patient, but at the expense of a rise in false activations," Dr. Barnes said in an interview.
"We’re the only group I know of that has examined this trend over time, but while presenting this poster a lot of interventionalists who came by said that they’ve seen it too," said Dr. Barnes, a cardiologist at the University of Michigan, Ann Arbor.
Now that they have identified the problem, Dr. Barnes and his associates believe there is a way to address the false-activation issue without compromising rapid responses. The key, they believe, is giving more consideration to each case and gauging the likelihood of a real STEMI rather than knee-jerk activations.
"The system became ‘page no matter what,’ which initially made sense, but maybe now we can finesse it a bit" and continue to have rapid responses without taxing resources as much, he said.
"In our new algorithm, we say that when patients are highly suspicious, with clear symptoms and ECG findings, by all means activate. But when it’s questionable, call and ask for a cardiology consult first; you don’t have to activate the entire team. That’s the first step," Dr. Barnes said.
"Also, we have two [emergency medical] systems that feed into our hospital, and we find more false activations from one system than the other. They use different ECG machines that use different algorithms, so we have been in touch with the ECG manufacturers to try to change that. That should have a major impact, because the paramedics use it as their major barometer" for acute MI, he noted.
Dr. Barnes acknowledged that the plan to swap activations for cardiology consults will be tricky and require commitment.
"The problem is that, when [a paramedic or emergency physician] asks for a consult it takes time, but when you activate the cath lab everything else stops. Activating the cath lab has been the best way to get a cardiologist. What we are now doing is improving our access outside of acute MIs, for patients with chest pain who are not clear-cut STEMIs.
"If we can keep the average door-to-balloon time at 65 minutes or less I think we’ll be doing well, especially if we keep the number of patients with a time greater than 90 minutes very small," he said. On the false-positive side, "we have set a target of 20%," Dr. Barnes said. "We want to get all the STEMIs, and so we’re willing to have some false positives, but a 50% rate is not the right number."
Dr. Barnes said that he had no disclosures.