No one knows whether patients with stable ischemic heart disease and moderate or severe inducible ischemia benefit from revascularization when added to optimal medical therapy. A major, federally-funded trial named ISCHEMIA is underway to answer this question.
Main results from ISCHEMIA are still several years off, but the study has already produced an interesting finding about current cardiology practice and the way that cardiac stress-imaging studies are ordered.
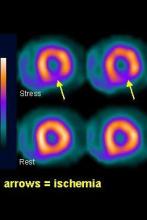 Courtesy Oliver Gaemperli and Phillip A. Kaufmann, University Hospital Zurich and the Society of Nuclear Medicine and Molecular Imaging
Courtesy Oliver Gaemperli and Phillip A. Kaufmann, University Hospital Zurich and the Society of Nuclear Medicine and Molecular Imaging
Main results from ISCHEMIA are still several years off, but the study has already produced an interesting finding about current cardiology practice and the way that cardiac stress-imaging studies are ordered.
Based on first-year enrollment data from the ISCHEMIA trial, the vast majority of both U.S. and European patients currently referred for stress-imaging assessment of ischemia have little or no inducible ischemia, Dr. Judith S. Hochman, head of the study, said during a talk at the American Heart Association’s Scientific Sessions in November.
Stable angina patients enrolled into ISCHEMIA need to have at least moderate inducible ischemia, defined as involving at least 10% of the left ventricle, in a cardiac imaging study read by a core laboratory. Since the trial began in July 2012, fewer than 700 patients had been enrolled based on imaging studies from about 15,000 patients. In the United States, about 3% of imaged patients had moderate or severe induced ischemia; the other 97% of patients referred for assessment had mild or no induced ischemia. In Europe, the rate with moderate or severe induced ischemia was slightly higher at 5%.
This observation made Dr. Hochman, a New York University cardiologist, ask why the prevalence of moderate or severe ischemia is so low in patients referred for stress imaging. She also wondered which patients with stable angina are undergoing revascularization today if so few qualify with moderate or severe inducible ischemia.
Another surprising fact she highlighted is how cardiologists manage patients found to have moderate or severe inducible ischemia. "Most of us think that all these patients with moderate to severe inducible ischemia are referred for catheterization," but that’s not what study results showed. She cited U.S. data from the mid- and late 2000s documenting that about one-third to two-thirds of these patients undergo cardiac catheterization.
This finding shows that there is "clinical equipoise" on how to manage these patients, and the ISCHEMIA trial will address that issue.
But until the results arrive in 2020, will as many stress-imaging studies continue for patients with stable angina when so many referred patients turn out to be negative for more advanced coronary disease? And, as Dr. Tracy Y. Wang, a cardiologist at Duke University, Durham, N.C., asked after hearing about the equivocal use of catheterization for patients with worse inducible ischemia: Why do physicians order these tests if they don’t intend to catheterize patients found to have moderate-to-severe inducible ischemia?
On Twitter @mitchelzoler

