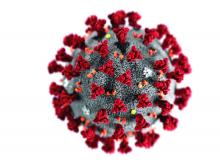
The novel coronavirus (2019-nCoV) is presenting a severe challenge to global health care, but its impact isn’t just felt in the emergency department. Specialists, including dermatologists, must also navigate the presence of the virus and its impact on patients and practices.
A new report from dermatologists in China’s Wuhan province, where the 2019-nCoV outbreak began, outlines initial experiences and provides a blueprint for triaging potential cases before they reach the dermatology clinic. Despite its presence in the epicenter of the outbreak, the hospital has not detected any 2019-nCoV-infected patients in any of its departments.
The commentary appeared in the British Journal of Dermatology and was authored by a group led by Juan Tao of Huazhong University of Science and Technology (Br J Dermatol. 2020 Mar 5. doi: 10.1111/bjd.19011).
The hospital triages all patients at the hospital entrance. Those who are suspected of having 2019-nCoV infection are sent to a designated department. Those with a skin condition who are not suspected of being infected are allowed to go to a dermatology triage center, where they are examined again. If the second examination raises suspicion, they are sent to the designated 2019-nCoV department. If no infection is suspected, or a patient from the 2019-nCoV department is cleared, they are allowed access to the dermatology clinic.
The team also suggested that skin lesions associated with dermatological conditions could lead to increased risk of 2019-nCoV infection. Contacted by email, Dr. Tao outlined a theoretical risk that the virus could lead to infection through contact with subcutaneous tissues, mucosal surfaces, or blood vessels. He did not respond to a request for evidence that such a route of transmission had occurred.
However, Adam Friedman, MD, professor of dermatology at George Washington University, Washington, said he doubted any such transmission would occur since the virus does not infect keratinocytes, and expressed concern that the suggestion could add to the stigma experienced by dermatological patients, whose noticeable rashes can sometimes lead to social avoidance. “I don’t want to add to that,” said Dr. Friedman in an interview.
A critical aspect of dermatology is the immunosuppressive agents often used in dermatology patients. Such drugs could make them more susceptible to infections, or to worse outcomes in the event of disease. Dr. Friedman recounted sending a letter to one patient on an immunosuppressive medication, suggesting that she work remotely. “I think that’s something we have to think about in at-risk individuals. I know there’s such a focus on the elderly, but there’s a large population of individuals on medications that lower their immune system who are going to be at risk for more severe infections,” said Dr. Friedman.
To reduce patient exposure, the commentary recommended that dermatologists perform online consultation for mild and nonemergency cases.
The authors also covered hospitalized patients with primary or secondary skin conditions. A dermatologist is on site at the dermatology triage station to conduct in-depth assessments if needed. If a patient has a fever that is believed to be caused by a dermatologic condition, the on-site dermatologist assists in the consult.
Because some patients may only become symptomatic after admission to a ward, the authors recommend hospitals have a COVID-19 trained contingency group on hand to prevent and control outbreaks within the institution. The team should be in communication with respiratory intensive care and radiology departments to exclude 2019-nCoV when cases develop in-hospital, and to ensure proper care infected patients who require it.
When a hospitalized 2019-nCoV-infected patient has a skin condition requiring treatment, the authors recommend that pictures be sent to the dermatologist for evaluation, along with teleconferences to further assess the patient. If necessary, the dermatologist should go to the patient’s bedside, with as much information as possible related in advance in order to minimize bedside exposure.
There was no funding source. Dr. Tao and Dr. Friedman have no relevant financial conflicts.