ANSWER
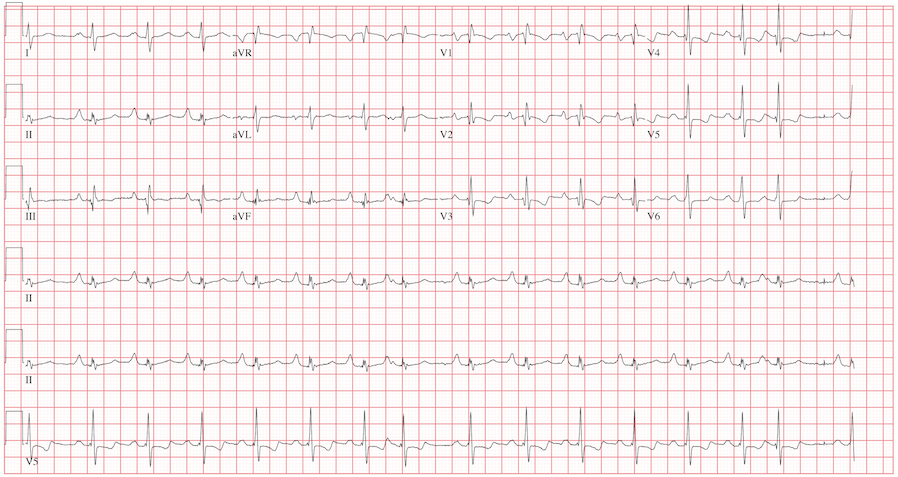
The ECG reveals sinus rhythm with a marked sinus arrhythmia, biatrial enlargement, incomplete right bundle branch block, right ventricular hypertrophy, ST and T wave abnormalities in the anterolateral precordial leads, and a prolonged QT interval.
There is a P for every QRS and a QRS for every P, and each P wave is similar in its respective lead (sinus rhythm); however, the rate is irregular, hence the diagnosis of marked sinus arrhythmia. Biatrial enlargement is illustrated by the presence of notched P waves in leads I and V1 with peaked P waves in leads II, III, and aVF (right atrial enlargement) and a P wave ≥ 110 ms in lead I with a terminally negative P wave ≥ 1 mm2 in V1 (left atrial enlargement).
An incomplete right bundle branch block is illustrated by the presence of an RSR’ in lead V1 with a small R and a QRS duration which is borderline normal (< 100 ms). Right ventricular hypertrophy is demonstrated by the presence of a tall R wave in V1 (in this case, R’) that is ≥ S wave in V1, an inverted T wave in V1, borderline right-axis deviation (R axis, 90°), and right atrial enlargement.
ST and T wave changes in the lateral leads are suggestive of anterolateral ischemia; however, in this case they are indicative of repolarization changes from right ventricular enlargement and an incomplete right bundle branch block. Finally, QT prolongation is suggested by the presence of a QT interval > 400 ms in a man when corrected for rate.
The patient’s history, physical examination, and ECG are highly suspicious for right-sided heart failure with the presence of jugular venous distention, a murmur of tricuspid insufficiency, hepatic congestion, and peripheral edema, as well as ECG documentation of right atrial and ventricular enlargement (cor pulmonale). An echocardiogram subsequently confirmed the diagnosis and also revealed pulmonary hypertension, with pulmonary artery pressures of 70 mm Hg.