Lastly, an individual’s ability (or inability) to metabolize calcium salts plays a vital role in the pathogenesis of stone disease. Intestinal calcium absorption is a major determinant of hypercalciuria, as nearly 90% of ingested calcium is absorbed in the intestines. People can broadly be divided into high or low calcium absorbers. Hypercalciuria (mean urinary calcium excretion ≥ 300 mg/d in men and ≥ 250 mg/d in women on a 1,000-mg/d calcium diet) is detected in 20% to 40% of those with calcium stones.21-23 Hypocitraturia (mean urinary citrate excretion ≤ 320 mg/d) and hyperoxaluria (mean urinary oxalate excretion > 45 mg/d) can also increase the risk for stone formation.12,24
Dietary Risk Factors
These are primarily related to fluid intake and dietary calcium.7,17,25,26 Drinking less than 1 L of fluids daily is associated with an increased risk for forming stones; this risk is magnified when the urine volume is also decreased.7,17,27 Increased dietary intake of animal protein can elevate the risk for formation of uric acid stones as a result of elevated urinary calcium and uric acid and decreased urinary citrate.17
Low dietary calcium ingestion and high oxalate consumption, resulting in increased oxalate absorption, can also exacerbate the risk for stones.7,27 By contrast, a diet high in calcium (≥ 1,200 mg/d) reduces the risk for calcium oxalate stone recurrence,17 although the effectiveness of supplemental calcium has been questioned.26-28
Patients who are advised to make specific dietary adjustments should later undergo repeat urine chemistries to determine the effectiveness of these changes.17
CLINICAL PRESENTATION
Nephrolithiasis typically presents with colicky flank pain, often accompanied by nausea and vomiting.29 The pain radiates to the ipsilateral groin, and the patient typically has difficulty finding a comfortable position. Nephrolithiasis may also present with chronic, episodic flank pain or may even be asymptomatic.30
Physical examination may reveal signs of severe pain, such as tachycardia and hypertension. Presence of fever indicates associated urinary tract infection and possibly pyelonephritis. Some larger stones can cause urinary tract obstruction; if obstruction occurs along with a preexisting urinary tract infection, it can potentially lead to pyelonephritis, pyonephrosis, and eventually urosepsis—a potentially life-threatening condition that requires immediate surgical drainage.31
Before a diagnosis of renal stones can be confirmed, care should be exercised to rule out the differentials, including abdominal aortic aneurysm, appendicitis, bowel obstruction, cholecystitis, drug-seeking behavior (eg, painkiller addiction), gastritis, mesenteric ischemia, musculoskeletal pain, ovarian abscess, ruptured ovarian cyst, pelvic inflammatory disease, pyelonephritis, and UPJ.2,32,33 All patients with suspected nephrolithiasis should be carefully evaluated using laboratory and radiologic investigations.
LABORATORY EVALUATION
The goals in this two-step process are to confirm the diagnosis of nephrolithiasis, then to identify the composition of the stones formed and the associated risk factors.
Initial Evaluation
Tests include dipstick urine assessment, serum chemistries, and a complete blood count (CBC). Urine dipstick assessment may be positive for blood, protein, or leukocyte esterase, indicating stones or fragments of stones present in the urinary tract. While nearly 10% of patients with stone disease exhibit gross hematuria, nearly 90% of patients have microscopic hematuria.2
Urine osmolality should be reviewed to assess urine concentration. Serum chemistries should be ordered to evaluate kidney function. Elevated creatinine may indicate acute rather than chronic kidney disease. Electrolytes and carbon dioxide should be measured to evaluate the kidneys’ ability to concentrate urine and maintain an acid–base balance. The CBC may reveal mild leukocytosis in nephrolithiasis; presence of significant leukocytosis indicates infection.2
Secondary Evaluation
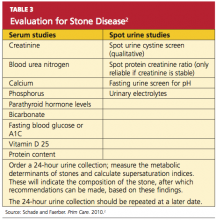
This step begins with a thorough review of the patient’s medical record and a detailed patient interview to ascertain all risk factors for stone formation (as summarized in Table 1). Specific studies to be considered are mentioned in Table 3.2 This evaluation is critical to prevent formation of future stones and the associated complications. In the patient with a history of stone recurrence or stone formation of identified cause, evaluation is needed for three metabolic abnormalities—hypercalciuria, hyperuricosuria, and hypocitraturia—as these conditions predispose patients to recurrent stone formation.1,25,34
The patient should also be encouraged to collect stones passed for further clinical evaluation. Infrared spectroscopy or quantitative wet analysis is used to identify the specific composition of the stone.32,35
Radiologic Evaluation
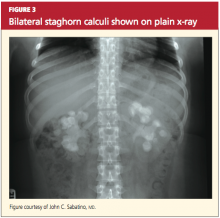
Radiologic evaluation of stones is currently performed through plain x-rays, ultrasonography, and noncontrast spiral CT.12,32,33 When a patient presents with acute signs of nephrolithiasis, a plain film x-ray of the kidneys, ureters, and bladder (KUB) is acceptable as the first imaging study, as it is inexpensive and available in most areas.33 Plain film KUB x-rays will identify calcium oxalate, calcium phosphate, struvite, and cystine stones. However, the sensitivity of plain film x-rays has been documented between 24% and 59%, and stones that overlie a bone may be missed.32,36 (See Figure 3.)