A 67-year-old man has a history of chronic dyspnea. He is a retired farmer who says he “never had time” to seek medical help for anything other than cuts or broken bones. In the past two months, he’s noticed that his dyspnea has progressively worsened. When questioned, he admits that his legs began swelling around that time as well.
Two days ago, he awoke from sleep unable to catch his breath. This morning, while walking to his mailbox, he became profoundly short of breath. He sat down by the side of the road and called 911. When the ambulance arrived, he felt much better but agreed to be taken to the emergency department, since his wife is away and he’s home alone. When questioned by the paramedics, he denied having chest pain, palpitations, productive or nonproductive cough, polyuria, polydipsia, nausea, or vomiting.
Medical history is positive for hypertension, gastroesophageal reflux disease (GERD), and hypertension. He has had several fractures in his right ankle and left femur, which are well healed. Surgical history is remarkable for a cholecystectomy and multiple laceration repairs on his arms and hands (also well healed).
His current medications include one aspirin per day and “a handful” of calcium carbonate tablets. Although he was prescribed “several heart pills” for hypertension, he hasn’t taken them or refilled the prescriptions for at least five years. He is allergic to penicillin and sulfa. He denies recreational or homeopathic drug use. He has never smoked, and he drinks one or two shots of bourbon on weekends.
Family history includes a father who died in a farming accident and a mother who died of cervical cancer at age 85. He has seven siblings, all of whom are alive and well.
The review of systems is remarkable only for GERD. Physical exam reveals a well-developed, obese male with a height of 6 ft 4 in and a weight of 278 lb. Vital signs include a blood pressure of 184/98 mm Hg; pulse, 90 beats/min; and respiratory rate, 20 breaths/min-1. He is afebrile. The HEENT exam is remarkable for atrophic glossitis. The neck shows no evidence of thyromegaly, and there are no carotid bruits or jugular venous distention. The chest is remarkable for diffuse wheezing and crackles in all lung bases.
The cardiac exam reveals a regular rate of 90 beats/min, with no evidence of murmurs, rubs, or gallops. The abdomen is obese. There is no evidence of ascites or masses. Evidence of 2+ pitting edema to the midcalf is present bilaterally. The neurologic exam is grossly intact, and the psychiatric exam reveals the patient to be alert and oriented, with a bright affect.
The working diagnosis in the emergency department is acute or chronic heart failure. A chest x-ray reveals moderate-to-severe pulmonary edema, cardiomegaly, and small bilateral effusions. Pertinent laboratory data include a serum glucose of 200 mg/dL and a B-type natriuretic peptide level of 590 pg/mL. All other lab values are within normal limits.
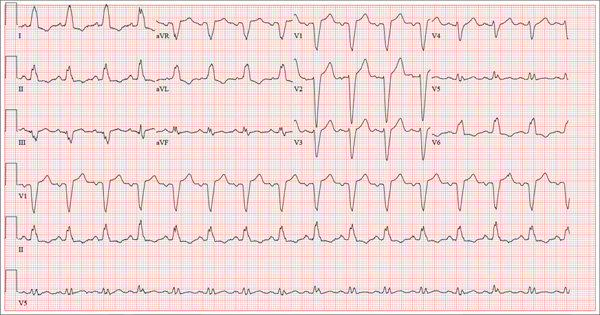
An ECG reveals the following: a ventricular rate of 93 beats/min; PR interval, 168 ms; QRS duration, 156 ms; QT/QTc interval, 430/534 ms;
P axis, 52°; R axis, 9°; and T axis, 171°. What is your interpretation of this ECG?