A 37-year-old white man presented to his primary care provider’s office for follow-up after a visit to the emergency department (ED). He had been evaluated at a local ED a week earlier for atypical chest pain and left arm pain. At the ED, blood work was done, along with an ECG, chest x-ray, and chest CT scan, but the results of these evaluations were not available during his initial primary care visit. On discharge from the ED, he was told that his heart was not the cause of his pain and that he should follow up with his primary care provider.
In the office, the patient reported that for the past several months he had been experiencing pain in his left arm when doing heavy or continuous physical labor; he noted that his job as a laborer required vigorous activity. Rest seemed to make his pain go away. He denied pain in the right arm or being awakened by the pain at night. Review of systems was unremarkable, and medical and surgical history was negative.
On physical exam, inspection of his torso and upper and lower extremities did not reveal any apparent abnormalities. Left shoulder and neck exams were normal. Cardiac auscultation was unremarkable, but palpation of the left upper extremity revealed neither a brachial, radial, nor ulnar pulse. Pulses in his right upper extremity were within normal limits. No bruits were appreciated over the carotids or either subclavian artery. Basic Doppler ultrasound over the left upper extremity at the brachial, radial, and ulnar sites showed symmetrical Doppler sounds. The remainder of his exam was unremarkable.
The patient’s ED documents and imaging results were received later in the day, after his office visit. The ECG, blood work results, and chest x-ray were normal. The chest CT results showed no evidence of pulmonary embolism. The radiologist did note mild narrowing at the left subclavian artery secondary to nonspecific surrounding soft tissue, which was noted to possibly represent intramural hemorrhage or atherosclerotic changes. No intimal flap was identified.
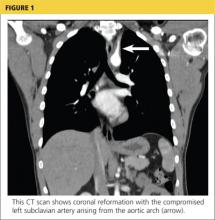
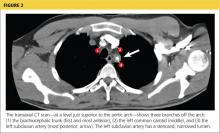
Because the diagnosis remained unclear, the patient was asked to bring the disc containing his chest CT images to the office. The radiologist, who was informed about the patient’s history and exam findings by phone, reviewed the CT images and felt there were changes surrounding the three branches off the aortic arch suggestive of inflammation, in addition to the stenosis at the left subclavian artery (see Figure 1 and Figure 2).
Based on the radiologist’s interpretation, additional lab tests were ordered. A complete blood count, comprehensive metabolic panel, prothrombin time/partial thromboplastin time, and lipid panel all yielded results within normal limits. Erythrocyte sedimentation rate (ESR) was 12 mm/h (reference range, 0 to 15 mm/h) and C-reactive protein (CRP) level was 4.9 mg/dL (reference range, 0.1 to 4.9 mg/dL). These laboratory results were essentially unremarkable, and therefore made his diagnosis more elusive.
The patient was referred to a vascular surgeon because of his immediate symptoms. The surgeon performed a thoracic outlet study in which Doppler waveform analysis of the left brachial, radial, and ulnar arteries of the thoracic outlet were analyzed during range-of-motion testing. Results suggested the possibility of thoracic outlet syndrome involving the left upper extremity, with significant baseline arterial insufficiency. A CT angiogram showed critical stenosis of the left subclavian artery and arterial wall thickening. Inflammatory changes were noted as well, and concern for “an inflammatory vasculitis” was described on the CT angiogram. The patient underwent left carotid-to-axillary bypass grafting, after which his left arm pain improved.
Following surgery, the patient returned to the primary care office for evaluation. Although the surgery was successful, the diagnosis was still not clear, requiring additional medical evaluation. The physical exam showed normal pulses in his left upper extremity. Lab tests revealed an elevated ESR of 54 mm/h and a CRP level of 4 mg/dL (reference range, 0.1 to 0.8 mg/dL; a different lab testing site was used, which accounts for the different reference range). In light of the patient’s lab test results, premature arterial vascular disease, and imaging studies suggesting inflammation, Takayasu arteritis (TA) was arrived at as a working diagnosis.
The patient was referred to a rheumatologist, who ordered a repeat ESR and CRP, antineutrophil cytoplasmic antibodies, and a magnetic resonance angiography study of the right brachial artery and major aortic branches to rule out other types of arteritis. Based on the test results, the patient was diagnosed with TA. He was placed on high-dose corticosteroid therapy (prednisone 60 mg/d). Methotrexate 10 mg/wk po was added three months after initiation of the prednisone.
Since being diagnosed with TA, the patient has presented with complaints related to the adverse effects of high-dose corticosteroids (ie, insomnia, weight gain, elevated blood pressure).
Continued on the next page >>