INITIATING CARE
Rapport is, of course, critical with all patients, but especially so in patients with HIV. The patient’s psychosocial as well as medical needs must be met in order to optimize adherence both to medication and to ongoing clinical care. HIV, even more than other life-changing chronic diseases, carries a stigma that patients can experience in a variety of ways. There are two messages that clinicians will want to convey to patients: HIV is a chronic, manageable condition, and support is available, either at the clinician’s office or through resources provided by the clinician upon diagnosis.
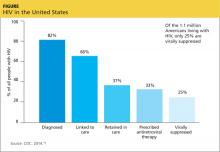
Underlying mental health problems, whether temporary or more chronic, can have a significant impact on the patient’s ability to adhere to the HIV treatment regimen. Addressing psychosocial needs may also help with patient adherence to clinical care. One of the most salient problems in HIV care today is retention in care. Only 25% of 1.1 million people living with HIV in the US are retained in care and achieve viral suppression (see Figure).18-20 Initial linkage to care and subsequent retention are areas in which all health care providers can play a role. Emergency and urgent care providers should have a protocol for immediate and direct referral of patients who test positive for HIV. Primary care providers can optimally treat their patients by closely monitoring response to therapy and reinforcing adherence to medication and to follow-up visits, both of which will substantially improve long-term survival.21,22
HIV treatment may begin as soon as the diagnosis is made and resistance test results become available, but the patient’s readiness to begin therapy is key. The patient needs to understand the chronic nature of the disease and the need for lifelong therapy so that he or she can commit to fully engaging in the management of the disease. While earlier HIV treatment improves the patient’s prognosis, the urgency of treatment increases gradually as the function of the immune system declines, particularly as the patient’s CD4 count drops below 350 cells/mm3.
The first step in managing a patient with HIV is to perform a complete history and physical examination. It must include a good family history; any concomitant medical conditions; current medications including herbal, alternative, and home therapies; and a complete social and behavioral history. Physical examination should be comprehensive, as manifestations of HIV may be subtle and can occur in any organ system. Physical manifestations of HIV are dependent on the patient’s immune status, but particular attention should be given to the skin and mucous membranes of the mouth and genitals as well as the neurologic examination. Neurologic complications of HIV may include sensory changes and cognitive dysfunction. Persistent nontender lymphadenopathy, which develops with initial infection, is frequently present. Of course, any clinical complaints should spur closer evaluation of the relevant system or systems.
Baseline laboratory testing should include confirmation of HIV if results were obtained anonymously or documentation is not available (Table 1). A resistance test (HIV genotype or GenoSure) should be performed at entry. Resistance mutations can be transmitted from person to person, and the baseline genotype offers the best opportunity to evaluate the patient for transmitted mutations. Resistance to a medication will determine antiretroviral therapy options for the patient. Hepatitis B and C status should be checked in all patients prior to starting therapy because results will impact therapeutic decisions. Patients co-infected with HIV and chronic hepatitis B should be evaluated by a specialist, since medication regimens for HIV and hepatitis B have overlapping activity against these viruses; it is generally advisable to fully treat both infections. Similarly, patients co-infected with hepatitis C and HIV should have a specialist consult. New advances in hepatitis C therapy are revolutionizing our approach to the disease, but HCV and HIV medications may have drug interactions.15,23
The most critical tests for evaluating the patient’s HIV status and response to therapy are the HIV RNA (viral load) and CD4 lymphocyte subset (also known as T cells, T4 cells, or CD4 cells). The CD4 count gives an estimate of the patient’s immune function, while the viral load is the best measure of the effect of medication. In general, the viral load should reach an undetectable level within the first few months of therapy. Other tests that should be done include chemistries and a urinalysis to evaluate renal function, liver enzymes, fasting lipids, and glucose (or A1C).
Other screening tests recommended at baseline include those for exposure to tuberculosis, toxoplasmosis, syphilis, gonorrhea, and chlamydia. Additionally, all women with HIV should have a baseline cervical cancer screening. Cytomegalovirus infection may be assumed in men having sex with men or injection drug users, but a screening immunoglobulin G antibody test should be done in patients at lower risk. Patients without a history of varicella-zoster virus infection or vaccination should be screened for that disease and may be considered for vaccination if they are older than 8 years with a CD4 count higher than 200 or ages 1 to 8 with a CD4 percentage higher than 15%.15,24 Additionally, a test for the HLA-B*5701 allele is recommended prior to starting a regimen containing abacavir. Performing this test at baseline will allow the patient and clinician a broader set of treatment options if the test is negative.
Ongoing monitoring of a patient with HIV depends on many factors. Early in treatment, it is important to keep a regular schedule of visits to monitor continued response to therapy. Additionally, clinicians should monitor for complications of HIV and its treatment, including renal and hepatic effects. Some medications used in HIV therapy can alter laboratory parameters with or without an effect on function. For example, atazanavir will often increase levels of bilirubin. The change is generally mild and not associated with clinical effects. Similarly, elvitegravir and dolutegravir both cause an initial increase in serum creatinine that has not, to date, been associated with clinical renal disease.
The most significant complications faced by patients with HIV as they age are cardiac, metabolic, renal, and bone disease that tend to occur earlier and with greater severity than in the general population. HIV medications are associated with osteoporosis, lipid abnormalities, abnormal glucose metabolism, and renal toxicity. Older patients and those with personal or familial risk factors should be monitored for these complications according to standard prevention guidelines. The new primary care guidelines for the care of patients with HIV published by the Infectious Diseases Society of America acknowledge the far more manageable nature of HIV and extended lifespan of those with the disease. The guidelines recommend extending follow-up intervals to every six to 12 months for those who have no other health complication and whose viral load is undetectable
(< 20 copies/mL) for two to three years.15,24
All patients should receive standard vaccines, including influenza (annually), Tdap (tetanus, diphtheria, pertussis), and human papillomavirus (ages 9 to 26 for females and 9 to 21 for males). In addition, patients with HIV should receive a pneumococcal vaccine and, if antibody negative, a hepatitis A and/or B vaccine.
On the next page: Initiating antiretroviral therapy >>