Second, perform baseline testing at the start of the season, then retest the injured athlete at set time intervals, charting improvement and rate of recovery. This serial assessment can provide a patient recovery curve for the clinician.30
Results from any neuropsychological testing protocol may be more valuable to the trained practitioner (usually a neurophysiologist, although developers of computer-based testing offer training and credentialing) than are subjective symptoms alone. However, clinicians must use these results as only one variable in the return-to-play decision.23 Cognitive testing is most reliable when baseline testing is included, but this may not be feasible in all settings. If baseline data are not available, normative data for the population of interest (eg, high school level) may be used; these are often available from the manufacturer of the computerized cognitive testing platform.
MOTOR CONTROL ASSESSMENT
Immediately following mTBI, a subtle yet significant degree of motor impairment may develop, often lasting beyond the acute phase of injury. This impairment may affect proprioception, fine and gross motor control, reaction time, and postural stability (balance), all of which are necessary and vital components of athletics. Any impairment in motor control will not only have a negative effect on athletic performance; it will undoubtedly increase the likelihood of a second and possibly more severe injury.
In the neurologic physical examination, results from the tests that are traditionally used to assess motor pathways and coordination have been subject to the individual clinician’s skill and interpretation.26 Several new tests have been developed to assess postural stability more objectively, producing data that give the clinician insight into the brain’s ability to organize incoming sensory information and respond appropriately to environmental changes.36 The gold standard for evaluating postural stability has been the force platform system, which measures vertical ground reaction forces as the body’s center of mass moves around a fixed base of support.26,37
This tool detects even minute alterations in the athlete’s postural stability as stress is exerted on the visual, vestibular, and somatosensory modalities; it can quantify the accuracy and timing of the subject’s motor responses. In recent studies of athletes with mTBI, vestibular and visual alterations caused a deficit in mean stability that peaked at 24 hours postinjury and lasted as long as 10 days before returning to baseline scores.36,38
Although performing force platform testing requires very little time, it is ordinarily administered by an otolaryngologist or an audiologist and usually requires a referral. Cost and limited accessibility make it impractical for obtaining baseline testing in entire teams or other large groups.
Compared with force platform testing, the Balance Error Scoring System (BESS)26 test has also been shown to produce reliable and valid assessments of postural stability.26,39 This low-cost alternative can be used in the clinic or on the sidelines to identify subtle impairments in postural stability, making baseline assessment for large groups feasible and helping clinicians safely return an injured athlete to play.
The BESS tests the athlete’s balance in three different positions, with eyes closed, on both firm and soft foam surfaces. Postural stability is determined by totaling the number of errors made during six 20-second trials (see Figure 2 and Table 3,26,39 page 21). Comparison studies have shown that athletes who experience mTBI have an increased number of errors on days 1 through 5 postinjury, compared with noninjured controls.36
DETERMINING RETURN TO PLAY
Despite the current emphasis on evidence-based practice and the possible consequences of premature participation in sports, the return-to-play decision often depends more on speculation than quantifiable data. The clinician is challenged to synthesize as much subjective and objective data as are available—patient-reported symptomatology, adjunctive assessment scores, and physical examination findings, and preferably with input from a management team that may include a certified athletic trainer, the team physician, a neurosurgeon, and a neuropsychiatrist.1,17
The student-athlete’s teachers should not be overlooked as observers of baseline classroom performance and possible dysfunction and impairment related to the injury. Parents and coaches may offer additional information, but the possibility of bias must be considered.
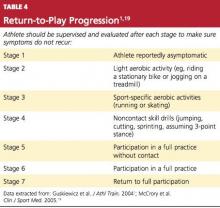
Only when the athlete reports that symptoms have fully resolved, it is generally agreed, should return to play even be considered.1,18,19 Then, provided that the athlete has regained at least baseline cognitive function and postural stability, a return-to-play progression can begin (see Table 41,19).
Athletes should be moved slowly through these stages, with ongoing supervision and reevaluation after each stage for possible recurrence of symptoms. On average, this progression takes three to five days.
CONCLUSION
No two mTBIs are alike. The mechanism of injury, the degree of neurologic dysfunction, and the time needed for recovery ultimately have no correlation. No athlete should return to play while mTBI symptoms persist, whether at rest or following exercise. If an athlete sustains an injury resulting in loss of consciousness (whatever the duration) or experiences amnesia, return to play that day should not be considered until further evaluation and/or neuroimaging can be performed.