MILD COGNITIVE IMPAIRMENT: HOW LIKELY THAT IT WILL PROGRESS?
Along with diagnostic criteria for AD, the NIA/AA developed criteria for a symptomatic predementia phase of AD—often referred to as MCI.14 According to the workgroup, MCI is diagnosed when
1. The patient, an informant, or a clinician is concerned about the individual’s cognitive decline from previous levels of functioning
2. There is evidence of cognitive impairment, ideally through psychometric testing, revealing performance below expectation based on the patient’s age and education
3. The patient is able to maintain independent functioning in daily life, despite mild problems or the need for minimal assistance
4. There is no significant impairment in social or occupational functioning.14
Progression: Less likely than you might think
Patients with MCI are at risk for progression to overt dementia, with an overall annual conversion rate from MCI to dementia estimated at 10% to 15%.15,16 This estimate must be interpreted with caution, however, because most studies were conducted prior to the 2011 guidelines, when different diagnostic criteria were used. Observers have noted, too, that the numbers largely reflect data collected in specialty clinics and that community-based studies reveal substantially lower conversion rates (3% to 6% per year).16 In addition, evidence suggests that many patients with MCI demonstrate long-term stability or even reversal of deficits.17
While there is some consideration of the use of biomarkers and amyloid imaging tests to help determine which patients with MCI will progress to AD, practice guidelines do not currently recommend such testing and it is not covered by Medicare.
WHEN EVIDENCE INDICATES AN AD DIAGNOSIS
When faced with the need to communicate an AD diagnosis, follow the general recommendations for delivering any bad news or discouraging prognosis.
Prioritize and limit the information you provide, determining not only what the patient and family want to hear but also how much they are able to comprehend.
Confirm that the patient and family understand the information you’ve provided.
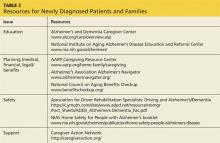
Offer emotional support and recommend additional resources (see Table 2).18
Given the progressive cognitive decline that characterizes AD, it is important to address the primary caregiver’s understanding of, and ability to cope with, the disease. It is also important to explore beliefs and attitudes regarding AD. Keep in mind that cultural groups tend to differ in their beliefs about the nature, cause, and appropriate management of AD, as well as the role of spirituality, help-seeking, and stigma.19,20
The progressive and ultimately fatal nature of AD also makes planning for the future a priority. Ideally, patients should be engaged in discussions regarding end-of-life care as early as possible, while they are still able to make informed decisions and express their preferences. Discussing end-of-life care can be overwhelming for newly diagnosed patients and their families, however, so it is important that you address issues—medical, financial, and legal planning, for example—that families should be considering.
Next: Medication for cognitive and behaviorial function >>