CHICAGO – Treating tattoos through a transparent perfluorodecalin-infused gel patch may cut down on the number of laser treatments needed to remove unwanted tattoos, results of a small pilot study suggest.
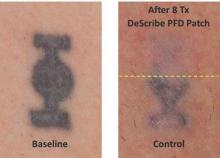
In 11 of 17 patients, tattoos treated through the perfluorodecalin (PFD) patch showed more rapid clearance of their tattoos compared with conventional treatment with the same 755-nm Q-switched alexandrite laser, Dr. Brian Biesman said at the annual meeting of the American Society for Dermatologic Surgery.
There were, however, a wide variety of responses, likely reflecting the heterogeneity of the tattoos themselves, ranging from no difference after many treatment sessions to more than 80% clearance after only two sessions, said Dr. Biesman, who is in private practice in Nashville, Tenn. Perfluorodecalin, a fluorocarbon that enhances oxygen delivery, reduces the epidermal whitening that typically limits Q-switched laser tattoo removal to a single pass. Use of the PFD patch in a prior study resolved whitening within an average of 5 seconds, allowing for three to four laser passes in less than 5 minutes (Lasers Surg Med. 2013 Feb;45[2]:76-80).
The DeScribe Transparent PFD Patch (ON Light Sciences) was approved in the United States in April 2015 for use as an accessory to laser tattoo removal procedures using a 755-nm Q-switched alexandrite laser in Fitzpatrick skin type I-III patients.
Anecdotal evidence presented by Dr. Biesman from his own patients suggests that the PFD patch may also speed tattoo clearance when used with different pulse durations and wavelengths, including 5-nanosecond (1,064 nm, 532 nm, and 650 nm) and picosecond (755 nm, 532 nm, and 1,064 nm) lasers.
“It does appear that this patch is efficacious with other Q-switched lasers, both nanosecond and picosecond,” he said, adding that this work is preliminary and under careful study.
The pilot study involved 17 patients with Fitzpatrick skin types I-III and black or blue tattoos treated with a conventional Q-switched alexandrite laser at the maximum tolerable fluence through the PFD patch on one side for three to four passes and with one pass through the air on the other side.
The patch allowed a factor of 1.5-times to 1.8-times higher fluence than control, Dr. Biesman said. In no case did the control side tattoo fade faster than the PFD patch side.
The study was sufficiently powered to qualitatively answer the question of whether the patch could enhance the clearance rate relative to control, but the quantitative rate could not be measured because of the small patient numbers, he noted.
Predictive factors were not identifiable because of the large number of variables, such as tattoo ink, tattoo location, and patient age.
There were no unanticipated adverse events with up to a year of follow-up. Three patients reported three areas of skin hypopigmentation that fully resolved, Dr. Biesman said.
The majority of patients in the pilot study, as well as in a 30-patient pivotal study, reported higher satisfaction with the patch treatment. This seemed to be from a combination of factors, including less discomfort during and after treatment, easier posttreatment recovery, and faster resolution, he said in an interview.
“In our practice, the patch has become the standard of care,” he added. “My nursing staff is highly protective of our patients and will not permit treatment of our patients without the patch. Based on our patients’ objective and subjective experience, I concur.”
Further studies to formally evaluate the performance of the patch in the treatment of benign pigmented lesions and with other Q-switched lasers, using a variety of wavelengths and pulse durations, are currently under consideration.