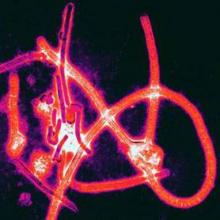
Separate groups of researchers supported by nonprofit and government agencies have assessed two novel Ebola virus disease treatments in the midst of the recent outbreak in West Africa.
The first study was a “natural experiment” that occurred when one Liberian treatment center temporarily ran out of first-line antimalarial drugs. This allowed investigators to discover that a second-line regimen may actually be more effective in reducing mortality from Ebola infection. (N Engl J Med. 2016 Jan 7;374:23-32. doi: 10.1056/NEJMoa1504605).
The lack of effective therapies against the Ebola virus spurred the U.S. Food and Drug Administration to identify several potential candidate treatments among compounds that are already used to treat other diseases, including malaria. However, there is little or no evidence to date concerning the real-world efficacy of these agents that have shown in-vitro activity against Ebola, said Etienne Gignoux of Epicentre, an epidemiologic research group headquartered in Paris, and of Médecins sans Frontières in Paris and Geneva, and his associates.
At the treatment center in Foya, Liberia, infected patients were routinely prescribed prophylactic antibiotics and a 3-day course of the antimalarial combination therapy artemether-lumefantrine, along with supportive treatment such as intravenous fluids. A 2-week shortage of this first-line antimalarial occurred during a sudden surge in admissions, and patients were instead prescribed artesunate-amodiaquine. Mr. Gignoux and his associates assessed outcomes in 194 patients prescribed artemether-lumefantrine, 71 prescribed artesunate-amodiaquine, 63 prescribed no antimalarials, and 53 for whom prescription data were missing.
They found that mortality risk was 31% lower with artesunate-amodiaquine than with the first-line antimalarials (risk ratio, 0.69). This mortality benefit persisted across several subgroups of patients, as well as in an analysis that specifically adjusted for the effects of potential confounding factors.
The results suggest that artesunate-amodiaquine may be preferable for the treatment of Ebola infection, but more research is needed to confirm this and to establish the safest, most effective therapeutic dose in these patients, the investigators said.They noted that their study had several limitations. The patient records included only prescribing information, so it was impossible to assess whether patients completed the full course of treatment. And all the antimalarials were oral formulations, so severely ill patients may not have been able to swallow or to keep down all doses.
In addition, artesunate-amodiaquine is known to cause more gastrointestinal adverse effects than the other antimalarials, so it’s possible that patients in that group were less likely to complete the full course of treatment. And many patients were concomitantly given the antiemetic metoclopramide, but data on possible adverse effects of this drug or possible drug interactions were not recorded.
The Liberian study was largely supported by Médecins sans Frontières, and the researchers reported no relevant financial disclosures.
Efficacy of convalescent plasma
In the second study, researchers at an Ebola treatment center in Guinea examined whether transfusion of convalescent plasma – plasma derived from patients who recovered from Ebola infection, which presumably carries helpful antibodies to the virus – was safe and effective. Their 6-month nonrandomized study involved 84 patients given two consecutive transfusions of 200-250 mL ABO-compatible plasma plus routine supportive care and 418 historical control subjects who had been treated before the plasma transfusions became available (N Engl J Med. 2016 Jan 7;374:33-42. doi: 10.1056/NEJMoa15118212).
The primary outcome – the risk of death during the 3-16 days after diagnosis – was 31% in the intervention group and 38% in the control group, a nonsignificant difference. This indicates that convalescent plasma transfusions do not exert a marked survival effect, at least at this dosage, said Dr. Johan van Griensven of the Institute of Tropical Medicine, Antwerp (Belgium), and his associates.
There were no serious adverse effects from the transfusions, and the procedure was acceptable to donors, patients, and caregivers.
The main limitation of this study was that actual levels of neutralizing antibodies in the transfused plasma could not be assessed. Such assays require biosafety level-4 laboratories, which are not available in the affected countries. “It is possible that high-titer convalescent plasma or hyperimmune globulin might be more potent” than the plasma used in this study, or that more frequent administration and higher total volumes could be more effective, Dr. van Griensven and his associates said.
They added that they “cannot exclude the possibility that some patients will benefit more than others from treatment with convalescent plasma.” For example, children younger than 5 years are known to be at high risk of death from the Ebola virus and had the highest risk of death in this study’s control group. However, four of the five patients in this age group who received convalescent plasma survived. Similarly, pregnant women infected with Ebola virus also are at high risk of death, but six of the eight in this study who received convalescent plasma survived.