Cosmetic Dermatology

Facial Rejuvenation: Combining Cosmeceuticals With Cosmetic Procedures
Cosmetic patients are looking for a more youthful appearance without spending a lot of money, feeling any pain, or experiencing any postprocedure...
From the Departments of Ophthalmology and Dermatology, Duke University Medical Center, Durham, North Carolina.
Dr. Woodward is a consultant for Allergan, Inc; Galderma Laboratories, LP; Merz Aesthetics; and SkinCeuticals. She also is a speaker for Galderma Laboratories, LP, and received grant support from Valeant Pharmaceuticals International, Inc.
Correspondence: Julie A. Woodward, MD, 3475 Erwin Rd, Durham, NC 27705 (julie.woodward@duke.edu).

Hyaluronic acid (HA) was first pioneered for use in humans in the late 1970s by ophthalmologists for anterior segment surgery.13-15 Biocompatibility for orthopedic and dermal applications was explored in the early 1990s.16
At this time, no dermal filler is approved by the US Food and Drug Administration for use in the periorbital area. Some fillers are approved for subdermal areas extending to the preperiosteal plane and can be used in the midface such as HA fillers (eg, Restylane Lyft [Galderma Laboratories, LP]), Juvéderm Voluma XC [Allergan, Inc]), poly-L-lactic acid (PLLA), and calcium hydroxylapatite (CaHA). No dermal fillers are approved for use in the forehead, glabella, or temples. Their use is becoming increasingly popular but is considered off label. In addition, cannulas are not approved for use in these areas. Cannulas may be beneficial in that they are thought to create less bruising and have less chance of entering a vessel than needles, but some injectors prefer needles because they are stiffer and therefore more precise.
The ideal filler for the tear trough, superior sulcus, ROOF, over the orbitomalar ligament, forehead, and glabella is one that is somewhat moldable but does not migrate, is not hydrophilic, is smooth to inject, and is reversible should there be any complications. No single filler fits this ideal description, but HAs typically are the first choice.
In vitro studies to determine the stiffness (G') and the ability to flow (viscosity) have been performed.17,18 Calcium hydroxylapatite has the most stiffness, while Belotero Balance (Merz Aesthetics) and Juvéderm Ultra XC (Allergan, Inc) are more soft17 (Table). These guidelines are important but may not correlate directly with how the fillers behave in vivo as demonstrated in animal models.18
An experienced injector is one who has developed not only an artistic eye for the face and excellent sense of anatomy but also has a sensitive ability to predict the filler-tissue interaction based on tactile feedback dependent on 3 main qualities: (1) stiffness and viscosity of the filler, (2) gauge of the needle or cannula, and (3) depth of the needle in the tissue. Periocular injections of dermal fillers can be delivered with needles or cannulas, diluted or undiluted. Smaller-gauge needles require more force than larger-gauge needles and cannulas that flow more freely. A needle in the dense dermis will require more force than one placed in the loose subcutaneous space.
The tear trough is generally preferable to fill with a mid-level G' HA filler that is less apt to migrate. A neutral gaze during the injection is preferred because closing or moving the eyes can distort the position of the inferior orbital fat-pads (Figure 1). A needle or cannula can be used, diluted or undiluted. The tear trough can be filled with the injection directed horizontally or vertically via a fanning technique. If needles are used, the skin should be stretched to view the 3 to 5 vertical veins and then the needle should be advanced beneath them to avoid bruising. Avoidance of hydrophilic fillers in the tear trough is important to avoid edema. The superior sulcus can be filled both anteriorly and posteriorly to the septum, which is a highly advanced injection for experienced injectors because of the proximity to the supratrochlear and supraorbital arteries as well as the superior ophthalmic vein (Figure 2). Sharp creases such as deep lateral periocular rhytides known as crow’s-feet are nicely filled with intradermal HAs with a low G'.
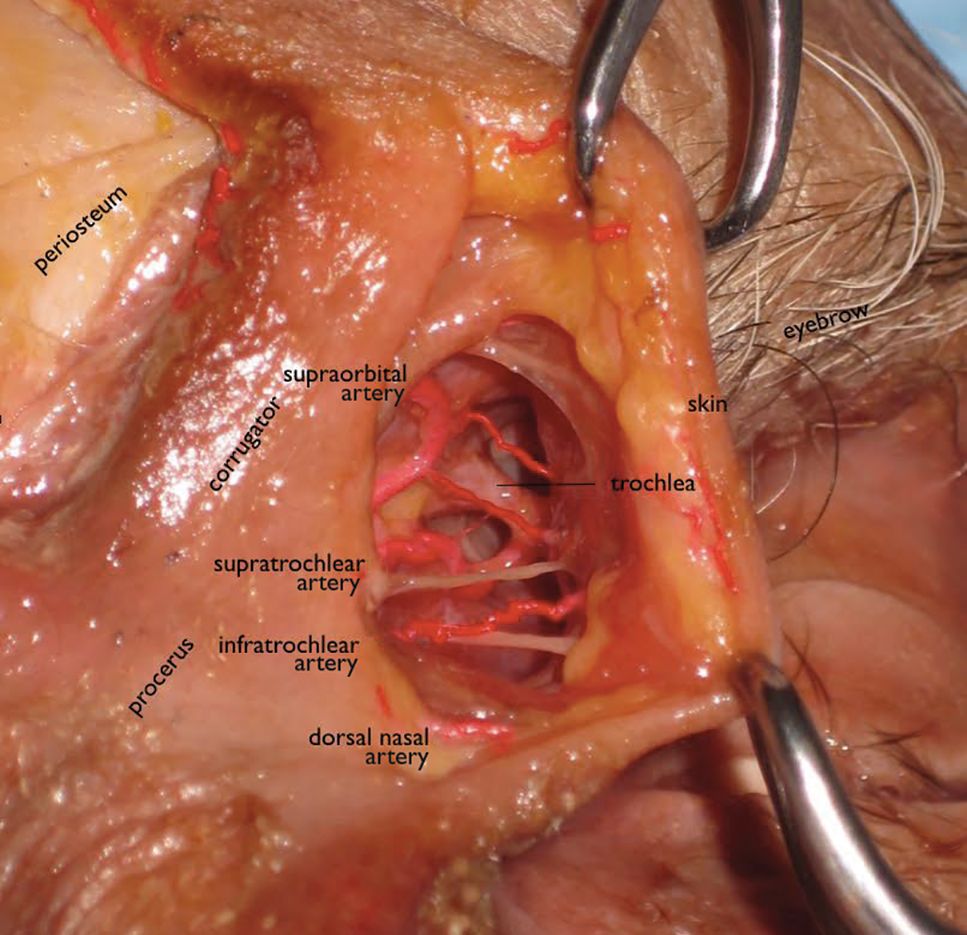 Image courtesy of Julie A. Woodward, MD.
Image courtesy of Julie A. Woodward, MD.
Figure 2. The skin of the glabella is deflected laterally so the corrugator and procerus muscles are left medially. The left superior medial orbit is exposed to show the large vessels in this area, making it the primary danger zone while injecting facial fillers.

Cosmetic patients are looking for a more youthful appearance without spending a lot of money, feeling any pain, or experiencing any postprocedure...

As part of our commitment to resident education, Cutis is excited to offer this monthly section with board-relevant, easy-to-review...

Vitiligo is an acquired idiopathic disease characterized by depigmented maculae and melanocytic destruction.
