VIENNA – Psoriasis in children and adolescents is associated with significantly increased risk of a variety of psychiatric comorbidities, according to a large Danish national study.
This finding has important public health implications. Psoriasis is a common skin disease, and 30% of cases have their onset in childhood or adolescence, Tanja Todberg, MD, observed at the annual congress of the European Academy of Dermatology and Venereology.
She presented a retrospective case-control study of prospectively collected national registry data on all children and adolescents diagnosed with psoriasis during 1997-2012. This amounted to 4,410 patients with a mean age of 12.4 years, 10.7% of whom had psoriasis sufficiently severe that they went on methotrexate. Each pediatric psoriasis patient was matched by age, sex, and calendar year with 10 controls.Diagnosis of psoriasis was based upon medical records and documentation that at least a second prescription for a topical vitamin D derivative had been filled. Those agents are the overwhelming choice as first-line therapy in the pediatric population, explained Dr. Todberg of the University of Copenhagen.
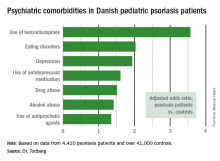
The pediatric psoriasis patients proved to be at significantly increased risk of being diagnosed with depression, eating disorders, drug abuse, and alcohol abuse. They were also more likely than controls to be prescribed antidepressants, antipsychotic agents, and benzodiazepines. That was every prespecified psychiatric outcome that Dr. Todberg and her coinvestigators included in the study except for one: anxiety disorders occurred at a similar rate in the pediatric psoriasis patients and controls.
Dr. Todberg said she undertook this Danish national study to confirm the earlier groundbreaking work led by Alexa B. Kimball, MD, professor of dermatology at Harvard Medical School, Boston. Those investigators showed in a large retrospective study of U.S. medical claims data that pediatric patients with psoriasis were at 1.25-fold increased risk of developing psychiatric disorders, with depression leading the way (J Am Acad Dermatol. 2012 Oct;67[4]:651-7).Dr. Todberg reported having no financial conflicts of interest regarding this study, which was supported by Danish medical research funding.