Case Letter

Telmisartan-Induced Lichen Planus Eruption Manifested on Vitiliginous Skin
To the Editor:A 39-year-old man with a history of hypertension and vitiligo presented with a rapid-onset, generalized, pruritic rash covering the...
Drs. Eyler, Garib, and Swan are from Loyola University Medical Center, Maywood, Illinois. Drs. Eyler and Swan are from the Division of Dermatology, and Dr. Garib is from the Department of Pathology. Ms. Thompson is from Pritzker School of Medicine, The University of Chicago, Illinois. Dr. Dahiya is from the Department of Pathology, Edward Hines Jr. VA Hospital, Hines, Illinois.
The authors report no conflict of interest.
Correspondence: Jennifer T. Eyler, MD, Loyola University Medical Center, Division of Dermatology, Bldg 54, Room 101, Maywood, IL 60153 (jenthompson11@gmail.com).

Annular atrophic lichen planus (AALP) is a rare variant of lichen planus. The clinical presentation of AALP shows distinct atrophic plaques with elevated borders on the trunk and extremities. Histopathologic findings generally reveal a lichenoid dermatitis in active lesions with a distinct loss of elastic fibers in the center of the lesions. We report a unique case of AALP, which highlights the chronicity of the eruption. Our patient showed early signs of improvement with hydroxychloroquine and acitretin, suggesting a role for systemic therapy in the treatment of AALP.
Annular atrophic lichen planus (AALP) is a rare variant of lichen planus that was first described by Friedman and Hashimoto1 in 1991. Clinically, it combines the configuration and morphological features of both annular and atrophic lichen planus. It is a rare entity. We report a case of AALP in a 69-year-old black man. The clinical and histopathological presentation depicted the defining features of this entity with a characteristic loss of elastic fibers corresponding to central atrophy of active lesions.
A 69-year-old black man with a history of hepatitis C virus infection and hypothyroidism presented to the dermatology clinic with a pruritic rash on the trunk, extremities, groin, and scalp of 4 months' duration. He denied any new medications, recent illnesses, or sick contacts. Physical examination demonstrated well-demarcated violaceous papules and plaques on the trunk, extensor aspect of the forearms, and thighs involving 10% of the body surface area (Figure 1A). The lesions were annular with raised borders and central depigmented atrophic scarring (Figure 1B). The examination also revealed several large hypopigmented atrophic patches and plaques in the right inguinal region and on the dorsal aspect of the penile shaft and buttocks as well as a single atrophic plaque on the scalp. No oral lesions were seen. An initial punch biopsy was consistent with a nonspecific lichenoid dermatitis (Figure 2), and the patient was prescribed triamcinolone ointment 0.1% for the trunk and extremities and tacrolimus ointment 0.1% for the groin and genital region.
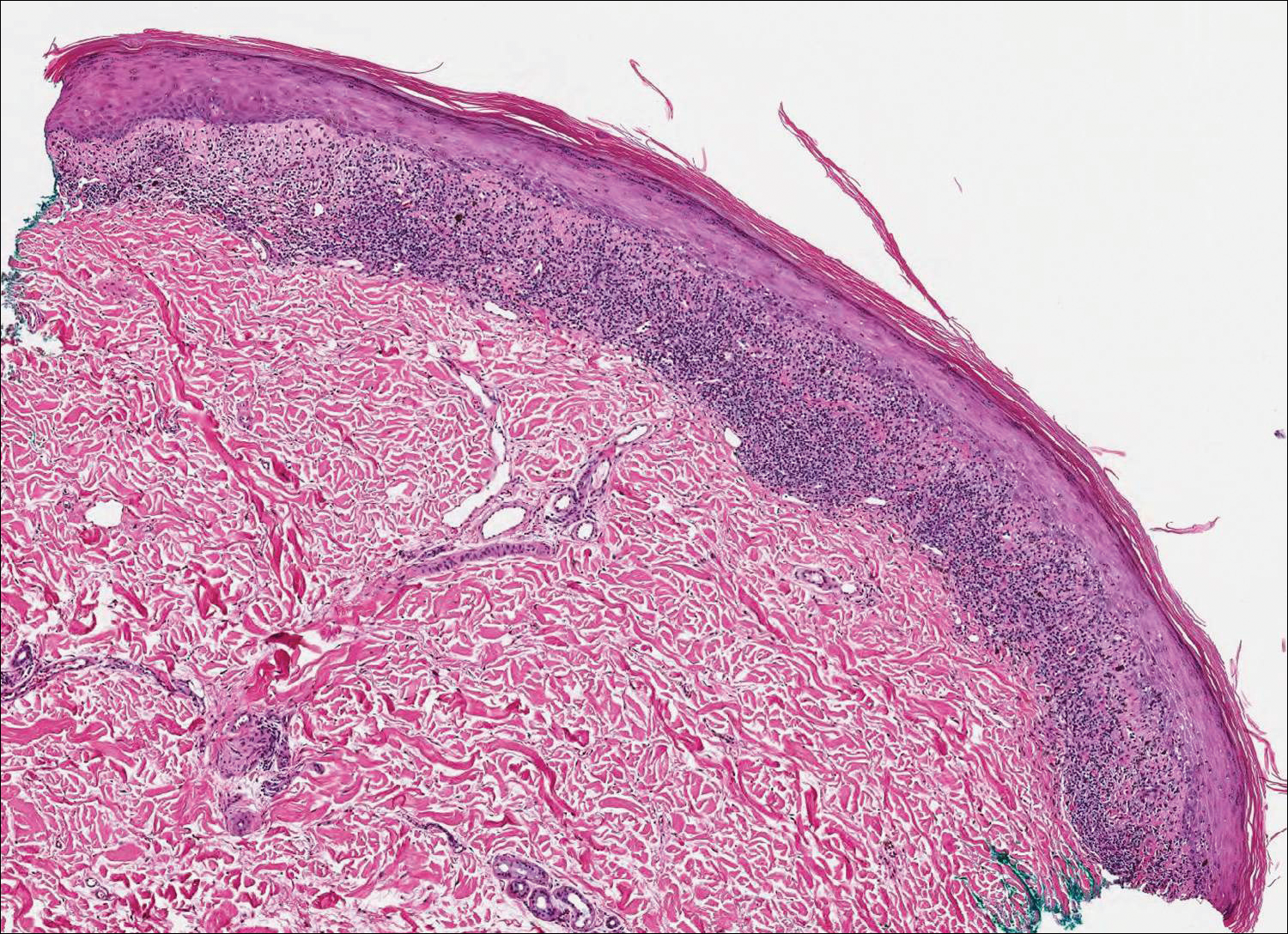
Figure 2. Punch biopsy from the left posterior thigh showed compact hyperkeratosis, hypergranulosis, Civatte bodies, and focal acanthosis with an underlying lichenoid dermatitis composed of a lymphohistiocytic infiltrate partially obscuring the dermoepidermal junction (H&E, original magnification ×40).
The patient continued to develop new annular atrophic skin lesions over the next several months. Repeat punch biopsies of lesional and uninvolved perilesional skin from the trunk were obtained for histopathologic confirmation and special staining. Lichenoid dermatitis again was noted on the lesional biopsy, and no notable histopathologic changes were observed on the perilesional biopsy. Verhoeff-van Gieson staining for elastic fibers was performed on both biopsies, which revealed destruction of elastic fibers in the central papillary dermis and upper reticular dermis of the lesional biopsy (Figure 3A). The elastic fibers on the perilesional biopsy were preserved (Figure 3B).
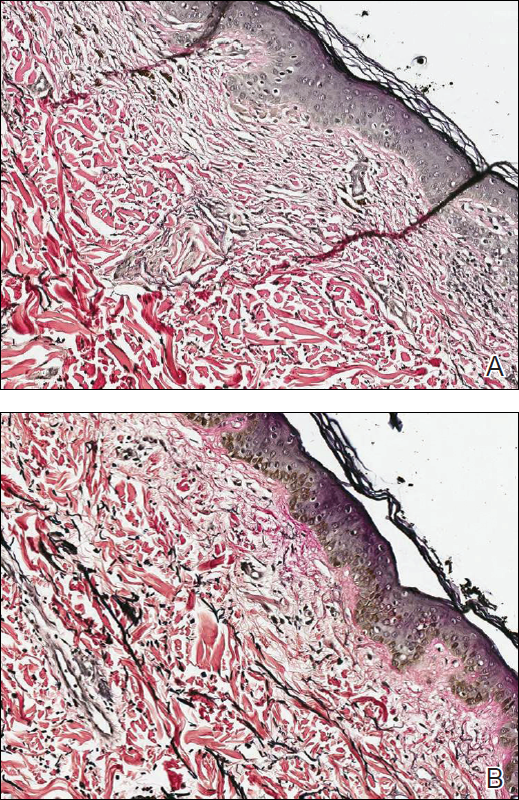
Figure 3. Verhoeff-van Gieson staining performed on a punch biopsy of a lesion from the upper back showed a decreased amount of elastic fibers in the dermis (A)(original magnification ×200). Punch biopsy of clinically unaffected adjacent skin was unremarkable with preservation of elastic fibers (B)(original magnification ×200).
The clinical presentation and histopathological findings confirmed a diagnosis of AALP. The patient was prescribed a short taper of oral prednisone, which halted further disease progression. The patient was then started on pentoxifylline and continued on tacrolimus ointment 0.1% with minimal improvement in existing lesions. These medications were discontinued after 3 months. Hydroxychloroquine 400 mg once daily was administered, which initially resulted in some thinning of the plaques on the trunk; however, further progression of the disease was noted after 3 months. Acitretin 25 mg once daily was added to his treatment regimen. Marked thinning of active lesions, hyperpigmentation, and residual scarring was noted after 2 months of combined therapy with acitretin and hydroxychloroquine (Figure 4), with continued improvement appreciable several months later.

To the Editor:A 39-year-old man with a history of hypertension and vitiligo presented with a rapid-onset, generalized, pruritic rash covering the...

Lichen planus pemphigoides (LPP) is a rare condition characterized by tense blisters that arise on lesions of lichen planus (LP) and on unaffected...

A 62-year-old woman with an extensive history of cutaneous and oral lichen planus (OLP) presented with gradual worsening of oral pain refractory...
